Calculated Need: Algorithms and the Fight for Medicaid Home Care
A Comparison of Five States’ Eligibility Algorithm
Miriam Osman, Emily Paul, Emma Weil
ReportFor a summary of this report, read the fact sheet here.
Executive Summary
In the United States, millions of elderly people and people with disabilities rely on Medicaid Home and Community-Based Services (HCBS) to meet their daily needs — from help bathing and getting dressed to support preparing and eating meals — as well as to work and to participate in their communities. While this is a federal program, it is largely administered at the state level. As part of implementing its HCBS programs, each state is responsible for designing its own rules and systems to determine which of its residents are eligible for HCBS benefits and how much home care they should receive. Every state uses automated tools as part of determining HCBS eligibility.
Automated eligibility determinations for home and community-based services are not designed to meet people’s needs. Rather, they are better understood as political and budgetary tools designed to control access to state-provided home care benefits. These determinations are tied to the federally mandated HCBS eligibility standard, known as the institutional level of care.
The institutional level of care requirement is a product of the historical moment in which it was created, when pressure from the disability rights movement coincided with the federal government’s goal of reducing the costs of long-term care. Replacing institutional care with home care offered the promise of responding to political demands while reducing the government’s overall costs of long-term care. Yet the promised cost reductions could only be achieved by keeping home care costs down and limiting home care to those who were in, or would otherwise be in, an institution.
Our work on automated HCBS eligibility determinations has led us to the following key findings:
The institutional level of care requirement and the algorithms used to enforce it, referred to in this report as LOC algorithms, are political tools that draw a subjective line between who is deserving and undeserving of receiving care in their home in an attempt to reduce the costs of long-term care.
Every state uses automated eligibility determinations for home-based care, and every state’s calculation of the institutional level of care looks different. Someone who is considered eligible for home and community-based services in one state may not be in many others. This variation across states emphasizes that these tools do not provide objective measurements of need but instead serve the policy and budget goals of the states’ HCBS programs.
States’ use of automated tools and reliance on private vendors depoliticizes the question of who deserves home care, obscuring it as a technocratic question of how to measure eligibility. States rely on four mechanisms that depoliticize LOC algorithms: (1) focusing on accuracy, (2) deferring to vendor expertise, (3) de-emphasizing the role of the algorithm, and (4) concealing assessments and algorithms from the public.
There are no “good” automated tools for HCBS determinations. While automated tools such as LOC algorithms can be tweaked to broaden eligibility, these tweaks alone, though often necessary for harm reduction, will not actually provide a path to fully meeting people’s needs. The only way people’s needs will be met is through creating a system of universal care in which elderly people and people with disabilities have the power to define their own experiences and articulate their own needs.
At the same time, we believe that an examination of LOC algorithms can provide an important window into the logic of eligibility determinations and provide an additional avenue for people with disabilities and their advocates to challenge individual determinations, as well as the broader system. In short, advocates should understand challenges to LOC algorithms as part of a bigger fight for a different system of care.
This report examines states’ use of LOC algorithms to determine eligibility for home and community-based services. The details of LOC algorithms are often shielded from the public in many states. Through public records requests and documents released by state agencies, we have nevertheless obtained substantial information about five jurisdictions: Mississippi, Missouri, Nebraska, New Jersey, and Washington, DC. We use these details to guide our argument that LOC algorithms are subjective political tools that vary across states.
We begin the report with background on the fight for home care led by people with disabilities and how we ended up with the institutional level of care as the eligibility standard. Next, we provide a basic explainer of how states determine eligibility, drawing on our comparison of the five LOC algorithms we obtained. We then examine the mechanisms state agencies and vendors use to depoliticize the question of who gets home care. Case studies on how Medicaid agencies in Washington, DC, Missouri, and Nebraska worked with vendors to define and implement the institutional level of care provide detailed examples of this depoliticization in practice. Finally, we offer recommendations for advocates on accessing and analyzing their states’ LOC algorithms. We hope this can support advocates in mounting challenges that build power through developing counternarratives and collective demands in collaboration with people directly impacted by LOC algorithms.
Collective challenges to state LOC algorithms can reduce harm in the short term, while helping to build the power needed to fight for universal care in the long term. This report aims to shed light on LOC algorithms and the eligibility determination process for advocates and people served through HCBS programs. Fighting for the changes needed to meet the needs of all will require the combined, coordinated, and concerted efforts of grassroots forces, legal aid organizations, advocates, people with disabilities, care workers, and many others. We hope this report is a useful step in identifying what we are up against in order to fight for the change we need.
Key concepts
Medicaid: Medicaid is a joint federal and state health insurance program for low-income people who meet both income requirements and other requirements based on their circumstances or needs. Medicaid is administered by states with a mix of state and federal funding. States develop their own Medicaid plans governing who will be covered, what services the state will provide, and how providers will be reimbursed. These plans must be approved by the federal government and are subject to federal requirements and guidelines. Medicaid is distinct from Medicare and largely covers different populations, though some people are eligible for both Medicare and Medicaid. At the start of 2025, roughly 71.2 million people were enrolled in Medicaid and 68.5 million were enrolled in Medicare, with 11.9 million enrolled in both programs.
Home and community-based services (HCBS): Home and community-based services refers to long-term care that is provided outside of a nursing facility or other institutional setting. It includes care in facilities such as adult day care and assisted living. A major component of home and community-based services is personal care, which includes assistance with things such as bathing, dressing, preparing and eating food, and taking medications, as well as with household tasks such as cleaning and grocery shopping. Anyone who qualifies for Medicaid is entitled to receive institutional care. By contrast, states are not required to create HCBS programs under Medicaid, meaning people who qualify for Medicaid are not necessarily entitled to home and community-based services beyond limited personal care services that are part of Medicaid state plans. There are two optional mechanisms through which states provide the majority of their home and community-based services: waivers and state plan amendments.
HCBS waivers: Waivers are one of the optional mechanisms for states to provide home and community-based services under Medicaid. HCBS waivers were established in 1981 as an amendment to the Social Security Act. They allow states to offer home and community-based services to specific populations and to provide different services to different groups by waiving federal Medicaid requirements for states to make the same services available to everyone who qualifies for Medicaid and to use the same income and resource eligibility standard across all programs. To qualify for an elderly and physically disabled waiver program, for example, an individual would have to meet additional functional requirements related to their needs, rather than just meeting Medicaid income requirements, and they may only be able to receive care in certain parts of the state.
Activities of daily living (ADLs): Activities of daily living encompass people’s basic needs, typically including things such as mobility, bathing, dressing, eating, and toileting. An individual’s functional needs are often assessed for HCBS eligibility based on the level of assistance they require to complete different activities of daily living. States may use different terminology to describe activities of daily living and instrumental activities of daily living (see below), with some state regulations describing certain tasks as the former where others will describe them as the latter.
Instrumental activities of daily living (IADLs): Instrumental activities of daily living refer to tasks that may require more complex thinking or organization and are critical to independent living, typically including tasks such as housekeeping, managing medications, managing money, cooking, shopping, transportation, and communication. The amount of assistance an individual requires to complete certain instrumental activities of daily living is sometimes included as part of an eligibility determination.
Institutional level of care (LOC): In order to be eligible for home and community-based services, individuals must be determined to require a level of care, or LOC, that would otherwise only be met in an institutional setting, such as a nursing facility or an intermediate care facility. There is a federal requirement for all states to carry out a face-to-face, standardized eligibility assessment for HCBS waivers to determine whether individuals meet the state’s institutional level of care requirement. Yet there is no standard definition for institutional level of care enforced across the country. Rather, it is up to each state to define the institutional level of care and to determine which activities of daily living, instrumental activities of daily living, and other factors (such as cognition, behavior, and medical needs) to include in the eligibility criteria.
Assessment: Any tool, such as a questionnaire or form, used by state agencies to gather information from people seeking home and community-based services to make eligibility determinations for HCBS waiver programs. These tools can take the shape of long questionnaires such as the interRAI Home Care (HC) assessment, one of the most commonly used assessment tools, or shorter forms designed by the state. Assessment tools are often created by vendors (private entities like interRAI, the American Association on Intellectual and Developmental Disabilities, Pearson, and others) and adapted to a state’s requirements, used off the shelf, or vendors may develop a custom assessment in concert with the state agency. Federal requirements mandate that the assessment be conducted face-to-face and be standardized.
LOC algorithm: An automated set of instructions, written by a state agency, typically with private consultants, that uses data collected from the assessment tool as input to make a determination about whether a person meets that state’s definition of the institutional level of care. LOC algorithms vary in terms of which assessment questions they consider and how they score the questions. LOC algorithms vary across states and have minimal regulations and testing. They do not measure a person’s need but instead measure whether a person meets the state agency’s definition of who is deserving of care under the federally mandated standard.
Automated tools: Any standardized tools or logic, including but not limited to LOC algorithms. This includes decision trees, spreadsheets, code, tables, instructions, algorithms, or guides used to make or inform decisions about access to care.
Institutional bias: Under federal law, the LOC standard used for HCBS eligibility must be the same as the LOC standard for nursing facility admission. The Supreme Court also has ruled that it is a violation of the Americans with Disabilities Act to unnecessarily institutionalize people who could receive care at home. In practice, however, it is much easier to qualify for nursing facility eligibility under Medicaid than it is to qualify for home and community-based services. And, once someone is found eligible, they are entitled to enter a nursing facility and have any services they need paid for by Medicaid. In contrast, even someone who has been found eligible for home and community-based services could be placed on a waitlist for years or could be given an insufficient budget to meet their needs at home. A study comparing nursing facility and HCBS assessment criteria found that the use of stricter criteria, more stringent methods of determining need, and longer assessment forms for home and community-based services in some states, as well as the longer timeframe and administrative burden these processes require, can limit access to HCBS programs, compared to access to nursing facilities. There is also less pressure to limit enrollment in nursing facilities for a variety of reasons, including systemic ableism (informing the fact that many people too readily accept that some people with disabilities “cannot” live in their own homes or communities, or would be too burdensome outside of an institution) and the fact that people’s desire to live at home instead of entering a nursing facility acts as a built-in limit on nursing facility enrollment. Finally, many people are pressured into entering nursing facilities, either because they are unable to receive the services they need through an HCBS program, because they are under guardianship and were not given a say, or because they were not informed of the array of services available to them. Together, these factors that favor placing people in institutions rather than providing access to care in homes and communities create what is termed institutional bias.
Cost containment: When the federal government expanded home and community-based services, it was under the rationale of “containing the rising costs of long term care.” State waiver programs are required to demonstrate cost neutrality, i.e., show that the waiver will cost the same as, or less than, the amount that would be spent on institutional care for the same population. Waiver programs are meant to cut costs by relying on so-called informal support (unpaid care provided by friends and family), reducing wages and benefits for care workers, and limiting access to the programs to only those who meet an institutional level of care requirement. At the same time, the government encourages privatization throughout Medicaid as an additional way of containing costs. Privatization is championed as a more efficient, cheaper option than publicly administered programs. But in reality, privatization is a way to get public funds into private pockets, while reducing avenues for accountability and transparency and cutting labor costs. The term “cost containment” is a euphemism for slashing budgets, underpaying workers, and scaling back public programs. It is strategic jargon that bureaucrats and industry experts use to make it seem like the government is doing something more sophisticated (and beneficial to the public) than it is.
I. Introduction
Disability benefits programs in the United States, including Medicaid Home and Community-Based Services, provide essential — though too often inadequate — support for people with disabilities. These programs often treat people with disabilities as untrustworthy and undeserving, as evidenced by restrictive and burdensome eligibility processes, severely limited benefits, and an emphasis on identifying individual fraud. These and other benefits programs are designed around the assumption that people are going to try “to take advantage” of the system — a racist and ableist idea that has deep social and historical roots in the United States. Benefits programs are also a product of class struggle. They were concessions won by workers and organizers for the benefit of all of society, and their systematic dismantling is an attempt to break the power of the working class and oppressed.
In July 2025, Congress passed sweeping Medicaid cuts that will strip away essential health care benefits from millions of people to fund the Trump administration’s tax cuts for the rich. While we still don’t know exactly how these cuts will affect home and community-based services, history has shown that they are a likely target. This significant attack on Medicaid coverage is part of a decades-long process — outlined, but by no means begun, in Project 2025 — to keep poor and working people barely at the threshold of survival, while the ruling class pockets the wealth of society. Welfare cuts are just one part of the story.
Further limiting who is eligible for benefits programs is one of the many ways these programs have been scaled back over time. State and private actors have built an extensive infrastructure of tools and technology to determine access to disability benefits. This infrastructure obscures the political decision to deny the right of people with disabilities to participate in society and replaces it with technocratic questions about measuring who should get benefits and how much they should get.
This report focuses on one example of this infrastructure: eligibility determinations for Medicaid Home and Community-Based Services for elderly people and people with physical disabilities. HCBS programs are the primary provider of paid home care for elderly people and people with physical disabilities in the United States. Access to Medicaid Home and Community-Based Services enables people to live in their communities instead of in a nursing facility or other institution.
Starting in the 1980s, states began expanding access to home care, driven by changes in federal policy. The disability rights movement was crucial to creating the necessary pressure on legislators to invest in home care for elderly people and people with disabilities. At the same time, federal policymakers were concerned about the growing costs of long-term care in institutions. Home care offered the promise of lowering those costs for the government, while also responding to grassroots pressure for these changes.
These two pressure points informed the eligibility logic for home and community-based services. Instead of universal home care, where everyone has a right to the care they need, the US system of publicly funded home care only treats people as “deserving” of paid care at home if their state determines that they require the amount of care that is provided in a nursing facility or other institution. The goal of limiting these services only to people who would otherwise be in an institution informed Congress’s statutory requirement for states to use an institutional level of care, or LOC, metric to determine eligibility.
Though it is federally mandated, the institutional level of care is not defined at the federal level. Every state defines its own level of care requirement through legislation, rulemaking, and the development of a LOC algorithm, typically built by private vendors. Our own and other research show wide variation in how level of care is defined and operationalized across states. This means, for example, that someone living in New Jersey might be eligible for home and community-based services in that state, but if they were to move to Washington, DC, they might not be. This system severely limits people’s ability to live where they want to live and still get the care they need.
State Medicaid agencies frame institutional LOC algorithms as tools that ensure the “right” people get approved for home care, based on a standardized measure. In this process, measuring whether someone meets the state’s definition of the level of care is equated with whether that person needs home care. In reality, however, level of care is a misnomer. LOC algorithms do not measure how much care people need but instead enforce the state’s definition of who deserves to receive care in their home. Using standardized assessments and LOC algorithms does not make deciding who should get home care objective or fair. It merely obscures what is actually a subjective and political exercise behind claims of technical expertise and the opacity of proprietary interests. In the process, the use of standardization and automated tools depoliticizes the question of who deserves care and hinders advocacy.
The goal of this report is to shift attention from the question of whether a LOC algorithm is good toward an understanding that there is no such thing as a good LOC algorithm. LOC algorithms may be more or less harmful, but they are never “good.” Ultimately, our vision is a system of universal home care in which the institutional level of care as a barrier to care is obsolete. In the meantime, we seek to reduce the harms of LOC algorithms while also building power to demand broader access to — and more comprehensive funding for — home care for everyone who needs it.
In what follows, we begin with an overview of the origins of the institutional level of care requirement in home and community-based services and how to think about eliminating it in the future. We then explain the technical aspects of LOC algorithms to provide an understanding of how states determine who is deserving of home and community-based services. With this deeper understanding of LOC algorithms in mind, we explore the ways in which states depoliticize HCBS eligibility. Using case studies of LOC implementations in Washington, DC, Missouri, and Nebraska, we illuminate the mechanisms that state agencies and vendors use to turn the political question of eligibility determinations into a technical one. Finally, we conclude this report with a number of advocacy tools that are intended to support advocates in accessing, analyzing, and challenging LOC algorithms.
Using standardized assessments and LOC algorithms does not make deciding who should get home care objective or fair. It merely obscures what is actually a subjective and political exercise behind claims of technical expertise and the opacity of proprietary interests.
II. Dismantling the institutional level of care
The federal government’s decision to use the institutional level of care as the eligibility standard for home and community-based services was a political choice to restrict access to benefits programs. The institutional level of care is an artifact of the historical moment in which it was created. It does not measure a person’s need but rather is a way to control who is eligible for care.
The disability rights movement was crucial to creating the necessary pressure on legislators to turn away from institutional settings and towards HCBS. Throughout the 1960s and 1970s, disability rights activists in the United States, inspired by the civil rights movement, organized and fought for equal rights and against discrimination, and struggled against the medical model of disability that informed the mainstream 20th century view of people with disabilities that relegated them to institutions. Within the broader work of disability rights activists from the 1960s to the 1980s, the deinstitutionalization movement exposed the appalling conditions under which many people with disabilities lived in institutions and fought to shutter the worst of these institutions. During roughly the same period, activists in the independent living movement created the first independent living centers, providing a disabled-led, community-based alternative to institutional care that supported greater autonomy and social integration for people with disabilities.
During this same period, Congress and the courts responded to dismal conditions and abuse in nursing facilities by increasing standards, regulation, and oversight. Congress also took initial steps to provide federal funding to states for home and community-based services. In the late 1970s, driven by concerns about the growing costs of long-term care, the federal government began planning a demonstration project to “test the cost-effectiveness of home and community-based services as a substitute for nursing home use.” In 1981, as part of the Reagan administration’s Omnibus Budget Reconciliation Act, Congress amended the Social Security Act to create HCBS waivers, initiating a program with funding incentives for states to expand access to home and community-based services.
The Reagan administration and the disability rights movement championed this expansion of home and community-based services for very different reasons. For people with disabilities and disability rights activists, expanding home and community-based services was a step forward in the provision of dignified and comprehensive care. These services would go on to improve the lives of millions of people with disabilities and elderly people, supporting them to participate in their communities.
For the Reagan administration, however, the promise of expanding home and community-based services was its potential to contain the rising costs of Medicaid long-term care expenditures. The federal government at the time was willing to allow people to access care in their own homes and communities so long as this option could further the government’s priority of reducing costs. The restrictive eligibility requirements, waitlists, and limited services that people trying to access home and community-based services face today are not inevitable, but rather reflect political choices and priorities made at a specific historical moment.
Ultimately, there was a tension between the government’s budget-slashing aims and the demand for home and community-based services from elderly people and people with disabilities (and their families) who needed care and wanted to receive it in their homes or communities rather than institutions with infamously abysmal conditions. Policymakers used the offensive term “woodwork effect” to refer to their fear that people who were not already in or about to enter institutions would “come out of the woodwork,” wanting government-funded long-term care once it was offered in the home. Similar to invocations of the “welfare queen,” the use of this term emphasized the racist and ableist class warfare that uses ideas of deservingness to make sure that nobody gets more than they “should.” Policymakers’ fear of the “woodwork effect” speaks to the belief, that persists today, that people receiving public benefits and people with disabilities are inherently untrustworthy and that HCBS programs need additional barriers to make sure that only those who are the most “deserving” of care are able to receive it.
Over forty years later, the logic of access to home and community-based services set out during the Reagan era persists. Using a restrictive definition of who deserves to receive care in their own home or community is just one of the tactics the federal government uses to keep Medicaid’s long-term care costs down. Other tactics the government uses include limiting eligibility, underpaying care workers, relying on unpaid care from family and friends, and reducing service hours. The effect is that care is denied to many people who need it. In this report, we focus on just one of these tactics: the creation of restrictive eligibility standards.
The requirement for an individual seeking home and community-based services to meet an institutional LOC standard is the main way states identify those eligible for benefits, while excluding anyone else from access to these services. While the introduction of HCBS waivers led to the expansion of Medicaid Home and Community-Based Services in states, this expansion was curtailed by the policy goal of replacing institutional care with home care, rather than making home care available to everyone who needs it.
In a universal health care system that provides long-term care to everyone who needs it, there would be no need for a binary eligibility determination, and thus no need for defining an institutional level of care. People could go through a care planning process, in which an assessment could be used to help identify the services they need and from which they would benefit, rather than using the assessment as input to a binary eligibility determination. Recognizing that resources are not infinite, this planning could even involve a prioritization process involving the person receiving the services, where individuals could choose what services they would like to prioritize for themselves.
This already happens to an extent today, through Medicaid’s benefit for children under 21, the Early and Periodic Screening, Diagnostic and Treatment. Unlike HCBS waivers, the Early and Periodic Screening, Diagnostic and Treatment program provides an array of mandatory home care services to children who need them and does not have restrictive access requirements. Arbitrarily cutting people with disabilities off from these services at age 21 and pushing them into waiver programs, rather than just providing a continuity of care, is a demonstration of the political choices made to restrict the provision of public benefits to the greatest possible extent.
It is important to note that without a political commitment to universal long-term care, eliminating the institutional level of care requirement will not solve the problem of restrictive access to home and community-based services. Rather, other tactics would simply replace the institutional level of care requirement, such as waitlists and limiting services through the care allocation and care planning processes.
Advocates already have a starting point for bigger fights for universal care through work they are doing to reduce the harms of LOC algorithms. Advocates should continue this harm-reduction work from the perspective that the institutional level of care is a political and budgetary tool rather than a legitimate measure of people’s needs. This orientation helps redirect energy from technocratic fights around making LOC algorithms fairer and toward engaging with eligibility determinations in the same way that states and vendors do — as a tool to accomplish policy goals.
In the next section, we dive deeper into how states determine eligibility for home and community-based services to give advocates a better understanding of the idea of the institutional level of care requirement as a political tool.
Advocates should continue this harm-reduction work from the perspective that the institutional level of care is a political and budgetary tool rather than a legitimate measure of people’s needs. This orientation helps redirect energy from technocratic fights around making LOC algorithms fairer and toward engaging with eligibility determinations in the same way that states and vendors do — as a tool to accomplish policy goals.
III. How states determine HCBS eligibility
Although the institutional level of care is a federally mandated standard, each state establishes its own definition of institutional level of care through state agency rulemaking. Through rulemaking, state agencies may define specific criteria and scoring, or they may simply set forth more general requirements, such as someone needing support on two or more activities of daily living. This process is subject to requirements for public notice and comment though it remains inaccessible for many people.
State agencies then contract with vendors to develop an automated eligibility determination process that implements the state’s level of care requirement. There are several types of vendors involved in the implementation of LOC algorithms:
Standardized assessment vendors, such as interRAI
Implementation vendors that build the scoring algorithms for those assessments, such as Optumas and FEI Systems
Consulting vendors that make recommendations about best practices (beyond technology) regarding waiver program design and LOC criteria in regulations, such as Mathematica, Mercer, and, again, Optumas
These vendors offer state agencies a rationale and the automated tools to determine who is eligible for home and community-based services. In doing so, these vendors often claim proprietary interests in the states’ assessment and scoring algorithms that hide these tools from public scrutiny.
Who defines the institutional level of care requirement for HCBS eligibility determinations?
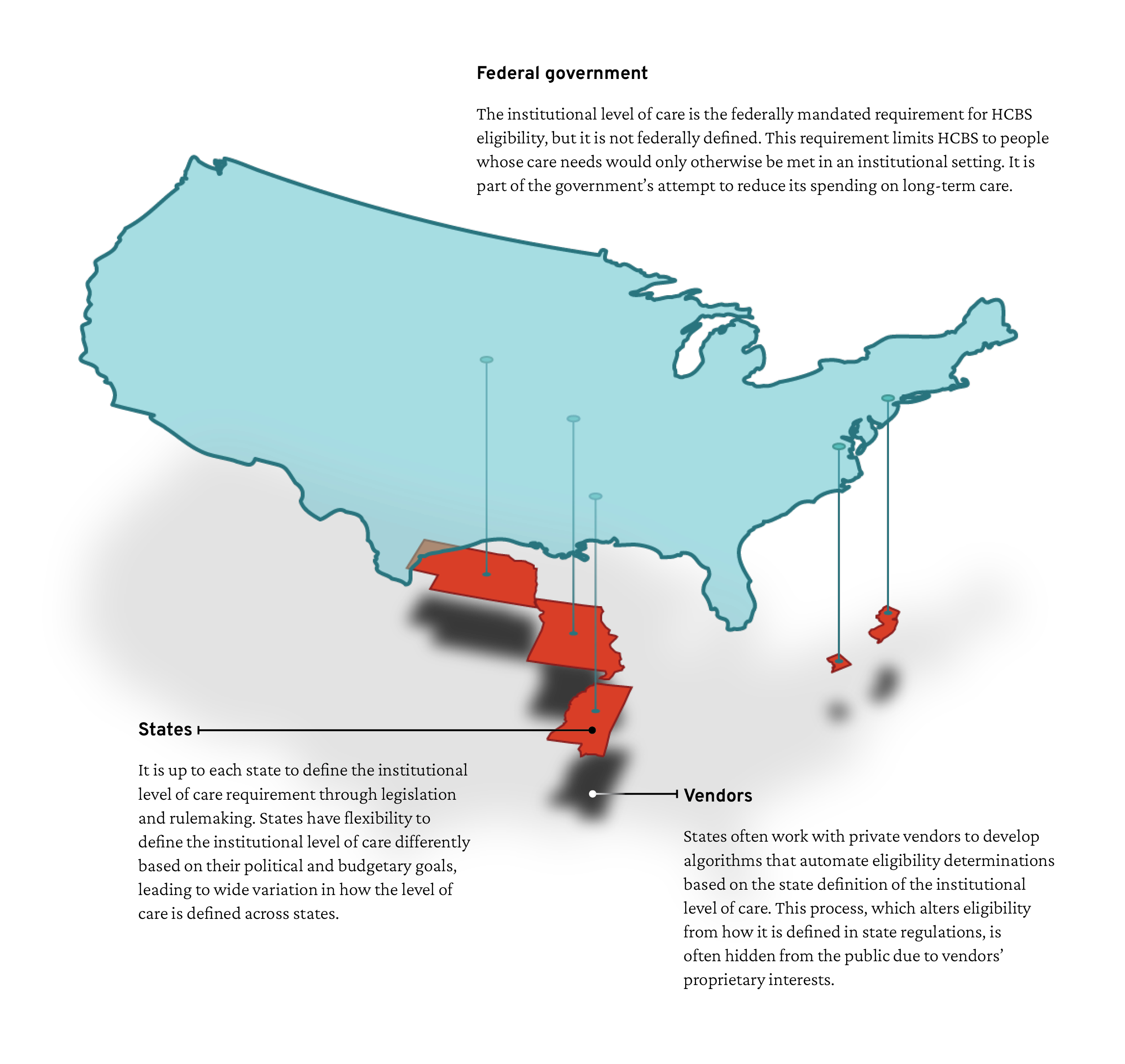
Who defines the institutional level of care requirement for HCBS eligibility determinations? This graphic illustrates how the institutional level of care is defined from the federal government down to states and their vendors. It shows the five states analyzed in our report, Nebraska, Missouri, Mississippi, Washington, DC, and New Jersey. The shadows below each state emphasize the opacity of most vendor-built tools.
Every state uses automated tools to determine eligibility for HCBS programs. Automated eligibility determinations can be broken down into two key steps:
A face-to-face standardized assessment to gather data: This is the step that is more visible to people applying for the program, their families and support people, and to legal advocates.
A LOC algorithm that calculates whether someone meets the state’s institutional LOC criteria: The algorithm is created by translating the LOC criteria in the state’s regulations into a set of instructions. This translation process often alters the criteria. Many people are not even aware that these algorithms exist and falsely perceive the standardized assessment as the determining factor for eligibility rather than the algorithm.
The eligibility determination process is largely hidden from public view, limiting opportunities for proactive advocacy or public engagement. Most people do not have insight into how automated determinations work for a variety of reasons, including vendors’ proprietary claims. States’ reliance on the private sector to create LOC algorithms further decreases transparency because these private entities are incredibly resistant to public scrutiny, are not publicly accountable, and deny the public access to basic information about their tools. Some of the most widely used assessments are developed by nonprofit research organizations, yet they still aggressively protect their proprietary interests.
Whether for- or non-profit, vendors tightly control information regarding how eligibility is determined. Even when the assessment or algorithm is created by the state Medicaid agency, it can still be difficult to access information about eligibility determinations. Our own public records requests from multiple states were denied on the basis of trade secrets exemptions and other barriers. Even when people access an algorithm, it can be difficult to understand what the algorithm actually does.
This section provides a baseline understanding of how institutional level of care is defined and operationalized. It draws on our analysis of documents obtained through public records requests and of HCBS waiver applications to explain how LOC algorithms are designed and used. In our research, we found a wide variation in how the level of care requirement is defined across states. This variation highlights that rather than being an objective measure of need, the level of care requirement and the automated systems used to measure it are political tools for states to control access to home and community-based services in line with their budget constraints and policy priorities.
The standardized assessment: Input for the algorithm
For people seeking services, the standardized assessment is the first step of the eligibility determination process. The assessments differ state by state, but they typically operationalize a medical understanding of disability that focuses on specific health and functional limitations, which allows few opportunities for individuals to contextualize or provide nuance regarding the support they require. For individuals, the assessment process can be burdensome, invasive, incredibly dehumanizing, biased in ways that make some disabilities less legible, and inaccurate in capturing a person’s actual care needs. How people answer a question on the assessment, what the assessor observes or believes the answer should be, or whether the person being assessed has a support person present can make or break whether someone receives the services they need.
Beyond the unavoidable limitations of standardization, there are myriad reasons why people’s assessments may not adequately represent their needs. People may not think about their capabilities on an average or bad day; may not remember things (such as when their last fall was); may overestimate their abilities; or may be too embarrassed to answer honestly. People also may not have a full understanding of what the possible responses to each question are and how they are used to determine eligibility. Assessors may also miss important information about a person’s needs due to oversight or bias, such as bias against particular forms of disability or based on race, gender, sexuality, or language. Overall, the assessment process can yield inadequate and inaccurate data as input for the LOC algorithm.
The interRAI HC assessment
The most widely used assessment for HCBS programs for elderly people and people with physical disabilities is the Home Care (HC) assessment created by interRAI, a vendor of assessments and algorithms that has been involved in automated HCBS determinations since the 1990s. As of 2024, the interRAI HC assessment is used in more than 25 different states. Over 100 million interRAI nursing home assessments have been completed in the US since 1990. Some states modify the interRAI HC assessment or other out-of-the-box assessments, and some design their own custom assessments. In this report, we focus on the interRAI HC assessment because it is widely used, including by the five states in our LOC algorithm comparison. Much of this analysis can be extended to other assessments and the interRAI HC is not unique in the issues it poses.
Figure 1. Functional Status Section of the interRAI HC Assessment
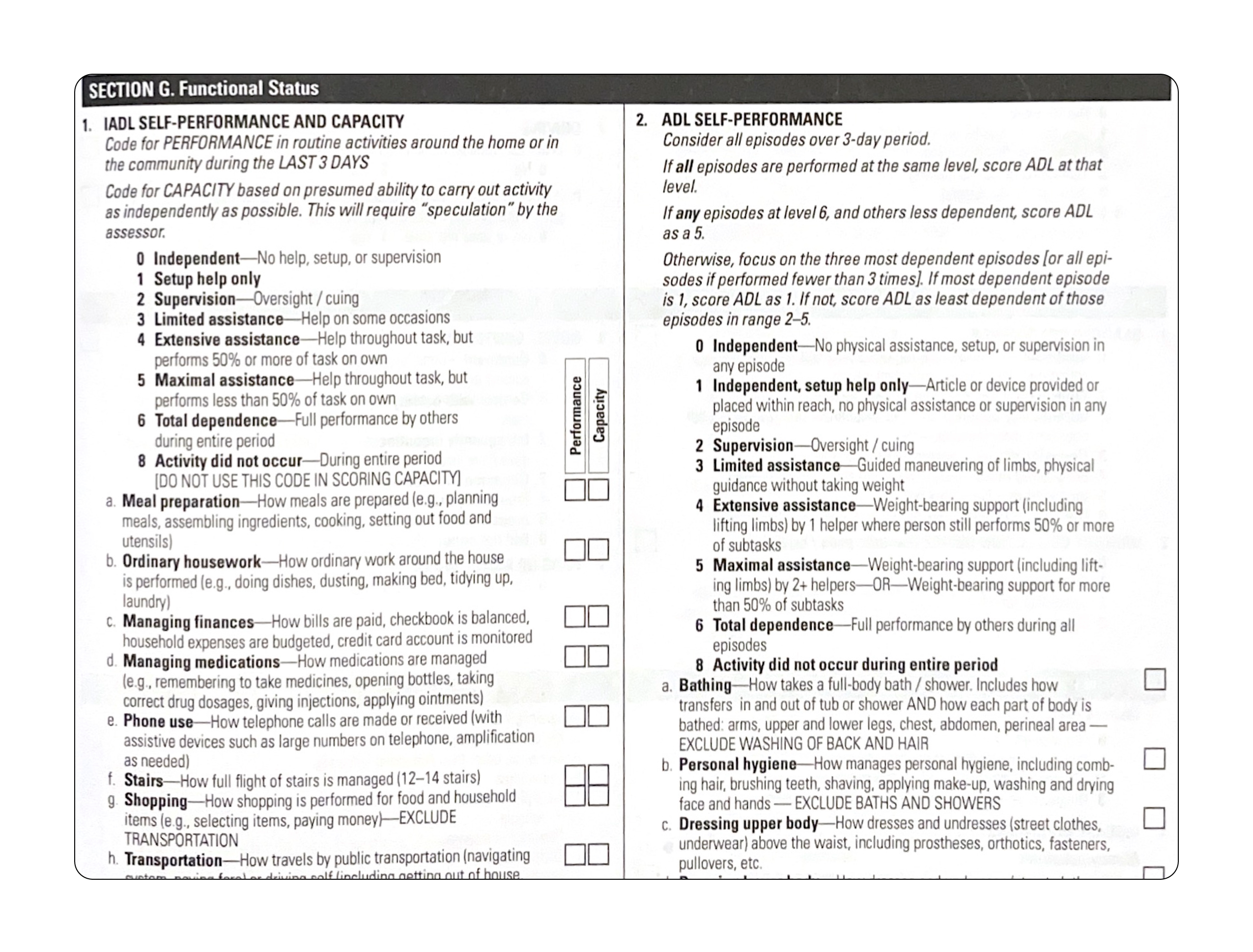
Figure 1. Functional Status Section of the interRAI HC Assessment. This figure, an example page taken from the widely used interRAI HC assessment, shows questions on instrumental activities of daily living and activities of daily living with scales for response options. Note the full list of activities of daily living is not pictured here because they continue on the following page of the assessment. Source: interRAI HC assessment form and user manual, standard English edition, version 9.1.
The interRAI HC contains more than 250 questions organized into 20 sections, including Functional Status, Continence, Treatments and Procedures, Health Conditions, Disease Diagnoses, Cognition, Communication and Vision, Mood and Behavior, as well as basic data gathering sections, such as Identification Information and Intake and Initial History.
States tend to rely the most on the Functional Status section in determining whether someone meets the institutional level of care requirement. The Functional Status section considers the support that people need with things such as eating, bathing, using the bathroom, and dressing (called activities of daily living, or ADLs) and with things such as grocery shopping, meal preparation, and medication management (called instrumental activities of daily living, or IADLs).
Figure 1 presents an example of the first page of the Functional Status section on the interRAI HC assessment form, and demonstrates how assessors translate an answer from someone seeking services into a numbered rating on an assessment and the potential response types on the interRAI HC assessment form. Some questions, such as the activities of daily living and instrumental activities of daily living shown in Figure 1, use ratings from 0–6 to quantify how much support the person needs for each activity: 0 if the person is able to do the activity completely independently to 6 if they are completely dependent on others to do the activity. If the person has not done one of the activities listed in the three days prior to the assessment, the person is rated an 8 (activity did not occur). In this report, we use the term “rating” to refer to the numerical values assigned to questions on the interRAI HC and the term “score” for how LOC algorithms use those values to determine eligibility.
Other questions on the interRAI HC have different rating options, such as those on the frequency of balance issues—from 0 (not present) to 4 (exhibited daily in the past 3 days—or bladder continence—from 0 (complete control) to 5 (no control present). Some questions, such as whether someone has pressure ulcers or other skin conditions, are rated as a binary, either 0 (not present) or 1 (present).
Many of the questions have what is called a “lookback period,” or a period of time prior to the assessment for which the assessor is supposed to consider the person’s needs. For activities of daily living and instrumental activities of daily living, for example, the assessor is instructed to score the person based on the highest amount of support that person needed in the past three days. Some questions have a longer lookback period, such as the question about falls, which considers whether the person has had a fall in the past 90 days.
According to interRAI, each of its assessment instruments, including the Home Care assessment, “represents the results of rigorous research and testing to establish the reliability and validity of items . . .” Reliability refers to a test’s ability to consistently produce the same results, whereas validity refers to how well the test measures what it is supposed to measure. There are multiple types of both reliability and validity.
One of the main measures used to demonstrate the reliability of the interRAI HC is inter-rater reliability. Inter-rater reliability is a measure of how similarly two different assessors score the same person on the same assessment. In practice, this metric is only able to tell us how consistently an assessment can be applied. Imagine an assessor comes to someone’s home and assesses them using the interRAI HC with its three-day lookback period for activities of daily living. This person may have fluctuating pain and mobility issues that did not flare up in the three days prior to the assessment, and as such, they might be assessed as not needing any support on activities of daily living. Yet if the assessment occurred on a different day, they would be assessed as needing support. This person could be assessed by two different people using the interRAI HC with the same results, resulting in high inter-rater reliability, while actually not fully capturing their needs.
Studies of the interRAI HC’s concurrent validity have measured alignment with established criteria. In this case, rather than comparing two different assessors using the same assessment, researchers looked at how similarly people were scored on the interRAI compared to previously established scales designed to measure needs for support and cognitive function and found what is considered “excellent agreement.”
To understand this measure of validity, imagine a scenario similar to the one outlined for reliability: An assessor comes to someone’s home and scores them on the interRAI, and a different assessor then assesses them using the other scales. The validity in this study is based on finding a strong correlation between the interRAI questions and those of the other scales. Even if neither measures the person’s needs well, this correlation could still be strong.
While there are numerous critiques of the reliability and validity of the interRAI HC and other assessments, we are primarily concerned with how state agencies and vendors act as if the reliability and validity of the assessment automatically transfers to their LOC algorithms. In reality, the algorithms are designed through a separate process and only factors in a subset of the assessment questions. By extending claims of reliability and validity from the assessments to the algorithms, state agencies and vendors fail to acknowledge the discretion involved in designing the algorithms. Most evaluations of the algorithms seem to be limited to analyzing their impacts on eligibility rates, which says nothing about the reliability or validity of the algorithm.
In reality, the algorithm is designed through a separate process and only factors in a subset of the assessment questions. By extending claims of reliability and validity from the assessments to the algorithms, state agencies and vendors fail to acknowledge the discretion involved in designing the algorithms.
LOC algorithms: Scoring the assessment to make an eligibility determination
The assessment on its own does not provide a determination about whether someone is eligible for home and community-based services under their state’s program. The way states use the assessment as input to determine HCBS eligibility varies significantly. When designing their LOC algorithms, state agencies and vendors may choose different subsets of assessment questions to include in eligibility determinations and assign different weights or scores to those questions and responses. As a result, even when states use the same assessment, their LOC algorithms can arrive at completely different conclusions. Simply knowing which assessment a state uses does not provide sufficient information to know how the institutional level of care requirement is operationalized. Despite the algorithm being crucial to understanding how the eligibility determination is made, states and vendors obscure their use of LOC algorithms and make them difficult to obtain.
Table 1.1. Comparison of Eligibility for Example HCBS Participant in Missouri
| Nebraska | New Jersey | Mississippi | Missouri | Washington, DC |
|---|---|---|---|---|
| Eligible | Ineligible | Eligible | Ineligible | Ineligible |
| Pathway 1 | Didn’t reach activities of daily living requirement for any pathways | 87.5 points (LOC = 50) | 9 points (LOC = 18) | 7 points (LOC = 9) |
Table 1.1. Comparison of Eligibility for Example HCBS Participant in Missouri. Source: Our LOC algorithm comparison is based on algorithms we obtained through public records requests and documents released by state agencies. See Appendix A.
To illustrate how different the scoring process can be across states, we examine and compare the use of the interRAI HC assessment in LOC algorithms in five states: Mississippi, Missouri, Nebraska, New Jersey, and Washington, DC. To understand how different choices state agencies and vendors make when designing an LOC algorithm can result in different eligibility determinations in different states, let’s look at an example scenario.
This example uses anonymized assessment data from someone who was receiving home and community-based services in Missouri and was then found ineligible when Missouri changed its LOC algorithm. According to their interRAI HC assessment, this person needs limited assistance with personal hygiene and dressing their lower body and needs set-up help for bathing, dressing their upper body, walking, and going to the bathroom. They need significant help with housework and shopping. They are incontinent, have consistent balance issues, and have severe pain and fatigue. They have been diagnosed with chronic obstructive pulmonary disease, congestive heart failure, coronary heart disease, diabetes, anxiety, and depression, and have had a stroke. This person had been receiving services in Missouri for years and expressed a desire to continue to receive services so that they could stay in their home.
Based on the same exact responses on the interRAI HC assessment, this person would be eligible for home and community-based services in Nebraska and Mississippi but ineligible in New Jersey, Missouri, and DC, as shown in Table 1.1.
This variation in eligibility has to do with choices that state agencies made in regulations and the choices the agencies and their vendors made in designing their LOC algorithms. Understanding these design choices and their impact on eligibility helps identify issues with these algorithms and potential ways to reduce their harms. The key design choices are:
Scoring approach: How an algorithm calculates eligibility. Based on our research, we have identified two distinct scoring approaches in LOC algorithms: The first is a “pathways” approach, in which a person is eligible if they fulfill the requirements for one of a set of predefined categories. The second is an “accumulation” approach, in which a person is eligible if they score enough points to meet or surpass the LOC threshold.
Questions considered: Which assessment questions are included in the algorithm at all. All LOC algorithms look at only a subset of the interRAI HC questions. In some cases LOC algorithms consider different questions based on what someone is rated on another question.
Scoring the questions: How ratings on interRAI HC questions translate into points or pathways in the algorithm. Both pathways and accumulation algorithms have minimum ratings below which a question is not considered. Accumulation algorithms add different amounts of points to the overall score based on question ratings. LOC algorithms can also give more or less weight to different interRAI HC questions. This means the algorithm can be designed so that questions that the state agency and vendor consider to be more important have more of an impact on whether someone is eligible.
We’ll now discuss each in turn.
LOC algorithms use different scoring approaches
A pathways approach only considers predetermined, mutually exclusive profiles of needs—that is, each pathway corresponds with a certain “picture” of need. Pathways can include, for example: people who need assistance in a certain number of activities of daily living; people who need supervision with activities of daily living and also have certain cognitive risk factors; people who need supervision with activities of daily living and have already been in an institutional setting; and people who need some help with activities of daily living and are elderly.
Table 1.2 compares the pathways and number of questions used to measure them in New Jersey and Nebraska’s LOC algorithms (the two states of the five we studied that use the pathways approach). Each numbered description in the list is a profile of someone who meets the eligibility criteria.
Table 1.2. Comparison of Pathways Algorithms
| State | New Jersey (three pathways) | Nebraska (four pathways) |
|---|---|---|
| Pathways | 1. The individual needs at least limited assistance in at least three areas of eligible activities of daily living. 2. The individual has cognitive deficits with daily decision-making and short-term memory, and needs supervision or greater assistance in three areas of eligible activities of daily living. 3. The individual has cognitive deficits with daily decision-making and making self understood, and needs supervision or greater assistance in three areas of eligible activities of daily living. | 1. A limitation in at least three activities of daily living and one or more medical conditions or treatments. 2. A limitation in at least three activities of daily living and one or more risk factors. 3. A limitation in at least three activities of daily living and one or more areas of cognitive limitation. 4. A limitation in at least one activity of daily living and at least one risk factor and at least one area of cognitive limitation. |
| Number of interRAI HC questions used | 11 (plus one custom) | 72 |
Table 1.2. Comparison of Pathways Algorithms. Source: Our LOC algorithm comparison is based on algorithms we obtained through public records requests and documents released by state agencies. See Appendix A.
Unlike the pathways approach, an accumulation approach is based on a person scoring enough points to meet or exceed the LOC threshold. Table 1.3 compares the number of questions, total possible points, and eligibility thresholds for the three states’ accumulation scoring algorithms in our comparison.
Table 1.3. Comparison of Accumulation Algorithms
| State | Mississippi | Missouri | Washington, DC |
|---|---|---|---|
| Number of interRAI HC questions used | 48 (plus 23 custom) | 57 | 31 |
| Total possible points | 408.5 | 129 | 31 |
| LOC Threshold | 50 points | 18 points | 9 points |
Table 1.3. Comparison of Accumulation Algorithms. Note: In Mississippi, a score between 45 and 49 prompts an additional review to see if someone should still qualify. Source: Our LOC algorithm comparison is based on algorithms we obtained through public records requests and documents released by state agencies. See Appendix A.
Neither of the two approaches described here is necessarily more inclusive. The questions a particular algorithm considers and how it scores the questions significantly impact its determination of whether someone meets a defined LOC pathway or points threshold.
LOC algorithms consider different assessment questions
Each state in our algorithm analysis uses a different subset of questions from the interRAI HC assessment to determine eligibility. While all five states include the majority of questions about activities of daily living from the Functional Status section, their algorithms are very different. Even in states that include the same activities of daily living in their algorithms, these questions are scored differently and there is significant variation in which, and how many, other interRAI HC questions are included.
Table 1.4. Questions Considered in LOC Algorithms
| State | Mississippi | Missouri | Nebraska | New Jersey | Washington, DC |
|---|---|---|---|---|---|
| Total number of interRAI HC questions used | 48 (plus 23 custom) | 57 | 72 | 11 (plus one custom) | 31 |
| Total number of sections used (out of 20 total) | 10 (plus one custom) | 11 | 13 | 3 | 5 |
| Number of activities of daily living (out of 10 total) | 8 | 9 | 9 | 8 (plus one custom) | 9 |
| Number of instrumental activities of daily living (out of 8 total) | 3 | 2 | 5 | 0 | 1 |
Table 1.4. Questions Considered in LOC Algorithms. This table compares data included in LOC algorithms by total number of questions and sections used and number of activities of daily living and instrumental activities of daily living used. Source: Our LOC algorithm comparison is based on algorithms we obtained through public records requests and documents released by state agencies. See Appendix A.
The number of questions included in the LOC algorithms in our comparison ranges from 12 in New Jersey to 71 in Nebraska. Table 1.4 includes a summary of the total number of interRAI HC questions and sections and the number of activities of daily living and instrumental activities of daily living included in the five algorithms in our comparison.
Table 1.5. Activities of Daily Living (ADLs) included in LOC Algorithms
| State | Mississippi | Missouri | Nebraska | New Jersey | Washington, DC |
|---|---|---|---|---|---|
| Bathing | • | • | • | • | • |
| Personal Hygiene | • | • | • | ||
| Dressing Upper Body | • | • | • | • | • |
| Dressing Lower Body | • | • | • | • | • |
| Walking | • | • | |||
| Locomotion | • | • | • | • | • |
| Transfer Toilet | • | • | • | • | • |
| Toilet Use | • | • | • | • | • |
| Bed Mobility | • | • | • | ||
| Eating | • | • | • | • | • |
Table 1.5. Activities of Daily Living Included in LOC Algorithms. Note: New Jersey’s algorithm includes one additional custom activity of daily living called Transfer. Source: Our LOC algorithm comparison is based on algorithms we obtained through public records requests and documents released by state agencies. See Appendix A.
None of the states in our comparison include all 10 interRAI activities of daily living. Three states do not consider Personal Hygiene, two states do not consider Bed Mobility, and three do not consider Walking. All five states, as shown in Table 1.5, include Bathing, Dressing, Locomotion, Transfer Toilet, Toilet Use, and Eating.
There is even less consistency in states’ use of instrumental activities of daily living in their algorithms, as shown in Table 1.6. New Jersey does not include any instrumental activities of daily living, and the only one included by all four of the other states is Managing Medications.
Table 1.6. Instrumental Activities of Daily Living (IADLs) Included in LOC Algorithms
| State | Mississippi | Missouri | Nebraska | New Jersey | Washington, DC |
|---|---|---|---|---|---|
| Meal Prep | • | • | |||
| Housework | |||||
| Managing Finances | • | ||||
| Managing Medications | • | • | • | • | |
| Phone Use | • | ||||
| Stairs | |||||
| Shopping | • | ||||
| Transportation | • | • |
Table 1.6. Instrumental Activities of Daily Living Included in LOC Algorithms. Source: Our LOC algorithm comparison is based on algorithms we obtained through public records requests and documents released by state agencies. See Appendix A.
Beyond the activities of daily living and instrumental activities of daily living in the Functional Status section, states vary significantly in which other questions their algorithms consider. Washington, DC, for example, does not include any questions from the Cognition section, while Mississippi considers seven questions from that section, Missouri considers five, Nebraska considers eight, and New Jersey considers two. Table 1.7 details a full list of interRAI assessment sections and which states include at least one question from each.
Table 1.7. Sections Included in LOC Algorithms
| State | Mississippi | Missouri | Nebraska | New Jersey | Washington, DC |
|---|---|---|---|---|---|
| Identification Information | • | ||||
| Intake and Initial History | • | ||||
| Cognition | • | • | • | • | |
| Communication and Vision | • | • | • | • | • |
| Mood and Behavior | • | • | • | • | |
| Psychosocial Well-Being | • | ||||
| Functional Status | • | • | • | • | • |
| Continence | • | • | • | ||
| Disease Diagnoses | • | • | |||
| Health Conditions | • | • | • | ||
| Oral and Nutritional Status | • | • | • | • | |
| Skin Condition | • | • | • | ||
| Medications | |||||
| Treatments and Procedures | • | • | • | • | |
| Responsibility | |||||
| Social Supports | • | ||||
| Environmental Assessment | • | ||||
| Discharge Potential and Overall Status | |||||
| Discharge | |||||
| Assessment Information |
Table 1.7. Sections Included in LOC Algorithms. Note: Mississippi’s algorithm includes additional custom questions not included in the counts above. Source: Our LOC algorithm comparison is based on algorithms we obtained through public records requests and documents released by state agencies. See Appendix A.
Some LOC algorithms use conditional logic so that the algorithm only considers certain questions based on someone’s rating on another question. In Missouri’s algorithm, for instance, if someone rates as having difficulty on the interRAI HC question on Making Self Understood, they only get points for that if they are also rated as having at least some level of difficulty on Cognitive Skills for Daily Decision-Making, as shown in Figure 2.
Which questions an algorithm includes is only one factor in who will be determined eligible for home and community-based services. While an algorithm that includes more questions might capture more types of need, that algorithm will not necessarily be more inclusive overall for HCBS eligibility since meeting a threshold or pathway also depends on how those questions are scored.
Figure 2. Cognition Section of Missouri’s LOC Algorithm
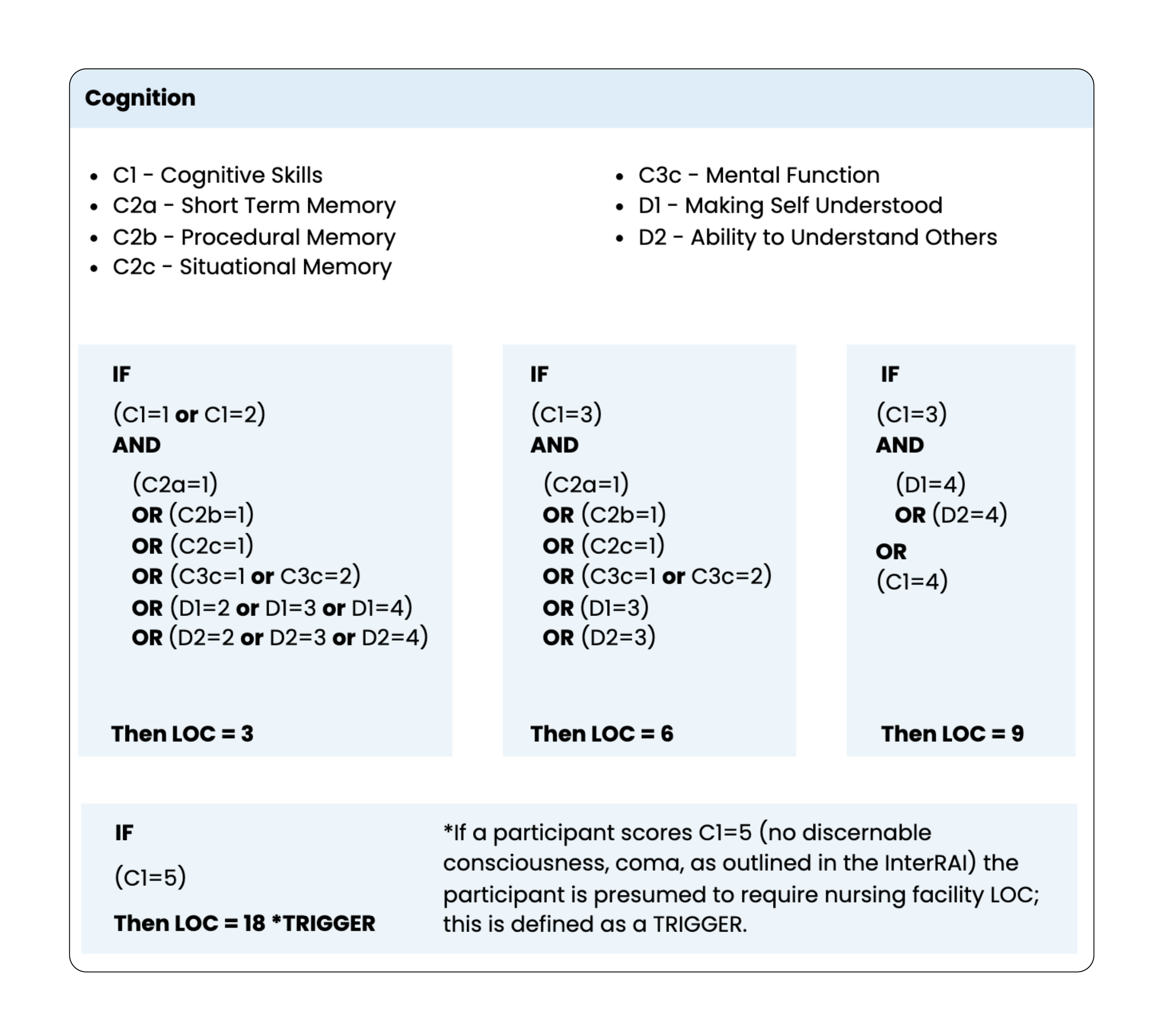
Figure 2. Cognition Section of Missouri’s LOC Algorithm. This figure shows the section on cognition in Missouri’s LOC algorithm, including which interRAI HC questions are included and how they are scored. Source: Missouri Department of Health and Senior Services, Nursing Facility Level of Care Algorithm, https://health.mo.gov/seniors/hcbs/pdf/loc-algorithm2-3.pdf.
LOC algorithms score questions using different minimum ratings and weights
In addition to deciding which questions to include and which scoring approach to use, states and their vendors have to decide how someone’s ratings on each assessment question factors into their eligibility determination. This includes setting a minimum rating on each question that determines whether to have the question factor in at all.
In Washington, DC, for example, if someone’s rating for an activity of daily living on the assessment is 1 (meaning they are able to do that activity independently after someone helps them set up) or higher (meaning they need more support), they receive points for that activity of daily living in the algorithm. Meanwhile, in Nebraska, any activities of daily living for which a person’s rating is less than 2 (meaning they need supervision to complete the activity) are not considered by the algorithm at all. And in New Jersey, activities of daily living are included if someone’s rating is a 3 (limited assistance) or higher unless they also have cognition issues, in which case their ADL needs are factored in starting at 2 (supervision). In Missouri, Eating is the only activity of daily living where a rating on the interRAI of 1 or 2 will get someone points in the algorithm, while for the other activities of daily living, a person can only get points towards the LOC score if the rating is a 3 (limited assistance) or above.
Eligibility determinations also depend on how a state’s algorithm factors specific questions into the overall score. State agencies and vendors can design the algorithm so that certain questions or sections have more weight, meaning those questions have more influence on the eligibility determination. They can also weigh different ratings on the questions differently.
LOC algorithms can use triggers so that a rating on a single question can make someone eligible. Missouri’s algorithm has several such triggers. The trigger logic for Mobility means that if someone is bedbound or fully dependent on others to move around, they receive 18 points on that question, making them eligible, as shown in Figure 3.
Figure 3. Scoring Logic for Mobility Section of Missouri’s LOC Algorithm
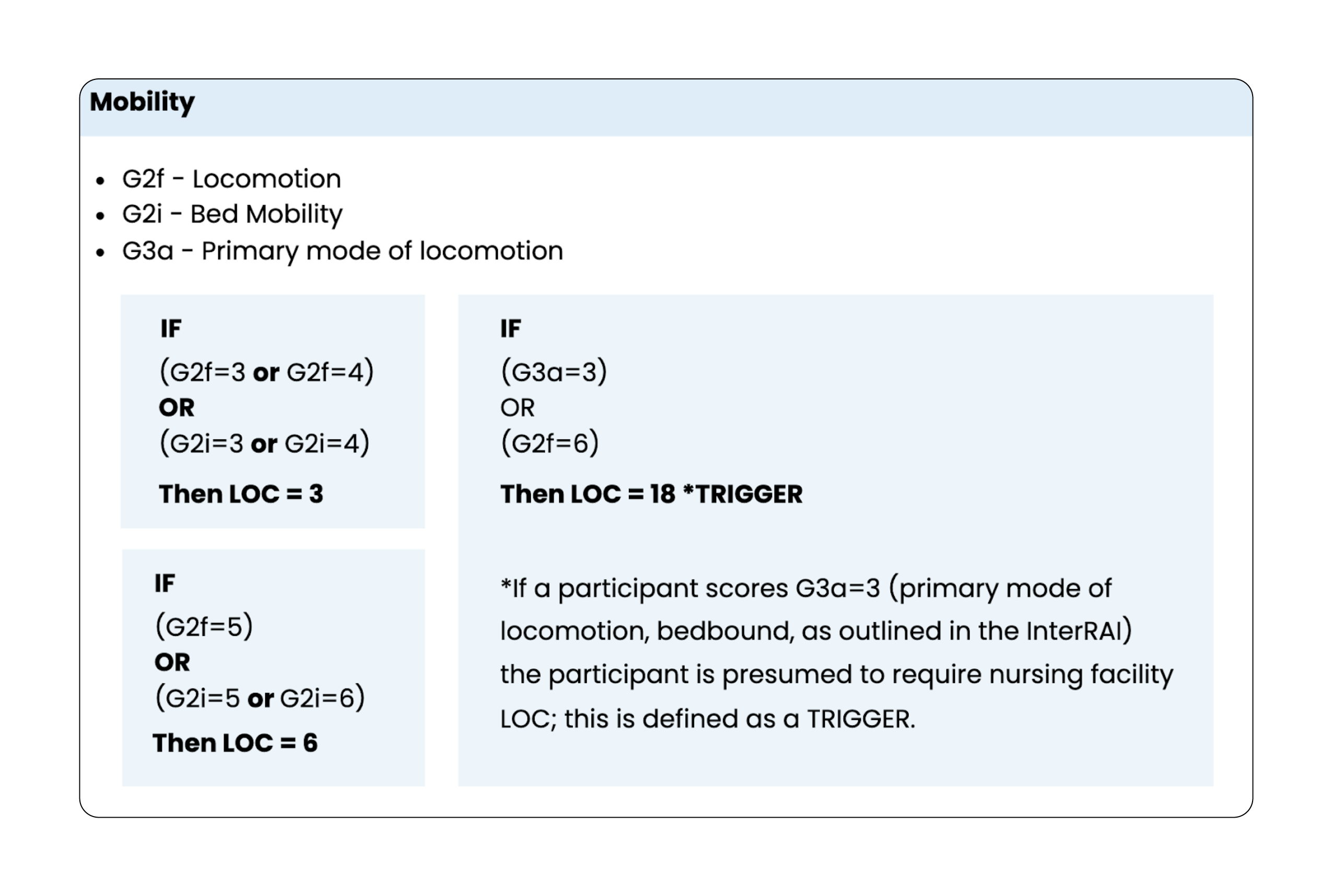
Figure 3. Scoring Logic for Mobility Section of Missouri’s LOC Algorithm. This figure shows the section on mobility in Missouri’s LOC algorithm, including which interRAI HC questions are included and how they are scored. Source: Missouri Department of Health and Senior Services, Nursing Facility Level of Care Algorithm, https://health.mo.gov/seniors/hcbs/pdf/loc-algorithm2-3.pdf.
Algorithm design choices can reflect the priorities of each state. Any of these algorithm design choices — from the scoring approach to the weight of different questions — can be used to achieve the state’s eligibility goals. For example, someone who needs limited assistance with three activities of daily living would be eligible in New Jersey but might not qualify if they moved to DC, where, based on the ADL questions alone, their score would be 3 out of the 9 points needed to be eligible. This is because in DC’s accumulation algorithm, an interRAI HC rating of 1, 2, or 3 on an activity of daily living only gives someone one point in the algorithm, whereas New Jersey’s pathways algorithm has an eligibility pathway for people who need limited assistance or higher on three or more activities of daily living. In DC for someone to be eligible based only on three activities of daily living, they would need to have a rating of 5 (maximal assistance) on all three. (See Figure 4.1 for the scoring of activities of daily living on DC’s algorithm and Figure 4.2 for the ADL pathway in New Jersey’s algorithm.) Understanding these design choices can help advocates analyze their state’s algorithm to identify what priorities it reflects about who the state sees as deserving of home and community-based services.
Figure 4.1. Activities of Daily Living Section of DC’s LOC Algorithm
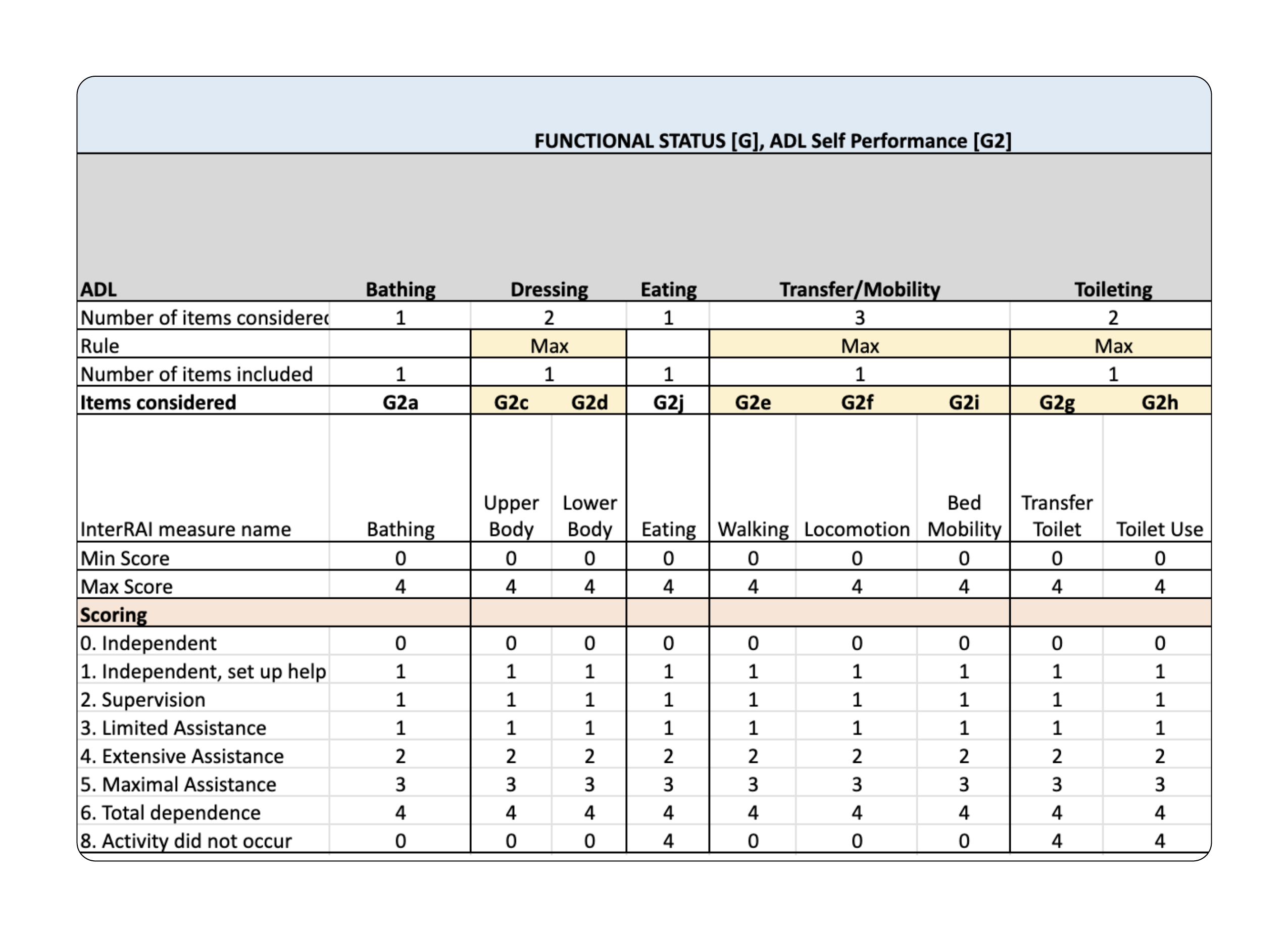
Figure 4.1 Activities of Daily Living Section of DC’s LOC Algorithm. This figure shows the activities of daily living included in DC’s LOC algorithm and how ratings on the interRAI HC translate to points in the algorithm. Source: Washington, DC, https://www.documentcloud.org/documents/26054260-interrai-hc-scoring-logic-dc/.
Figure 4.2. Activities of Daily Living Pathway in New Jersey’s LOC Algorithm
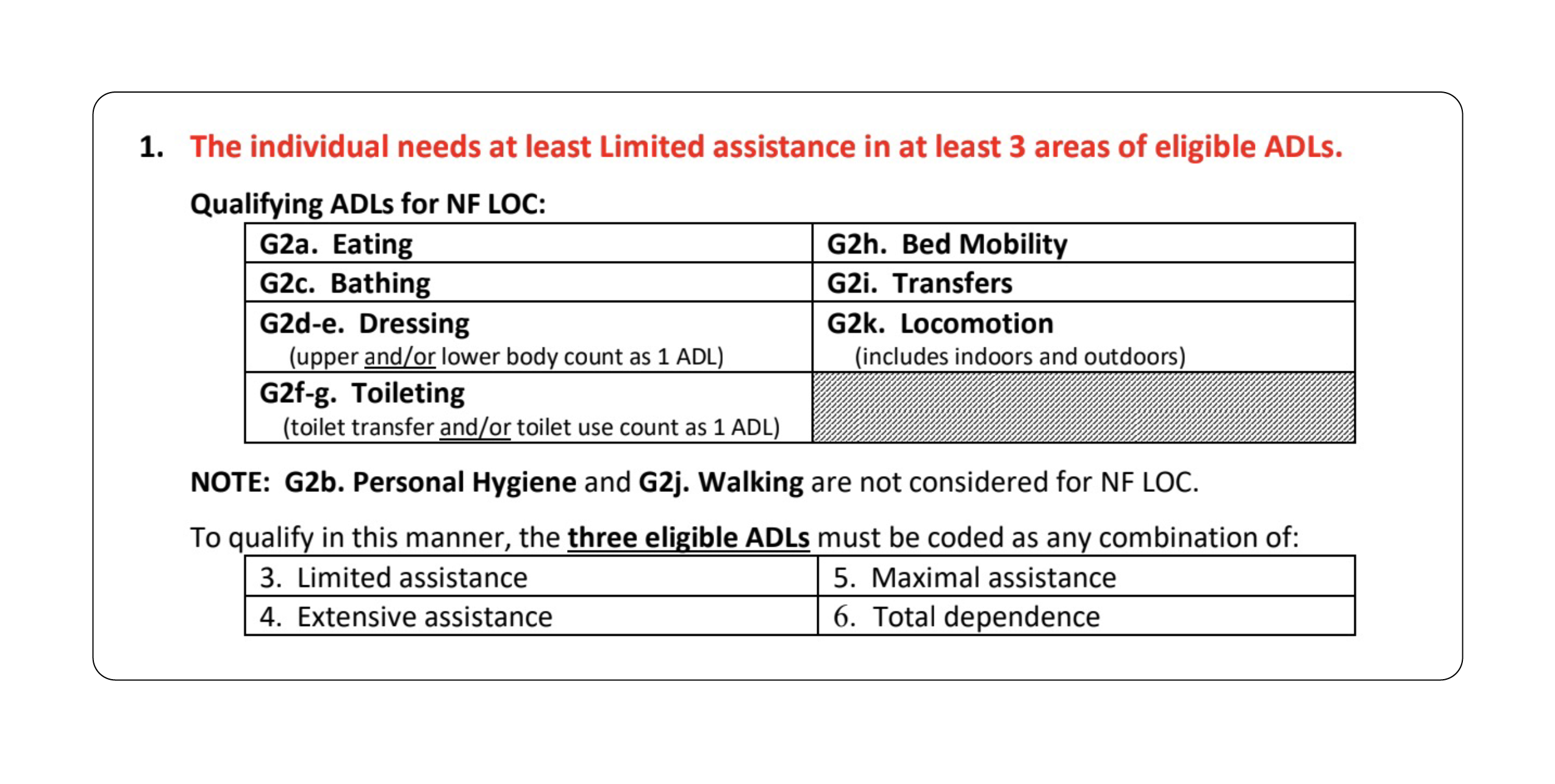
Figure 4.2 Activities of Daily Living Pathway in New Jersey’s LOC Algorithm. This figure shows the first pathway in New Jersey’s LOC algorithm which lists the activities of daily living and amount of assistance required to qualify. Source: See Appendix A, New Jersey, https://www.documentcloud.org/projects/222350-loc-algorithms-report-new-jersey/.
IV. How states depoliticize HCBS eligibility
The question of who is eligible to receive government-funded care is inherently political. When the federal government created HCBS waivers, it made a political choice to limit care to people who would otherwise be institutionalized. In implementing their HCBS programs, state agencies and their vendors end up reducing the political question of who deserves care to a technical question about how to define and measure institutional level of care.
States often talk about eligibility determinations as if there is an objective truth about who needs home and community-based services that can be uncovered through an objective process. The Missouri Department of Health and Senior Services, for example, stated that “this program will ensure the right services, to the right people, in the right setting, at the right time.” In Nebraska, one of the state’s vendors, Mercer, said that “a well-designed and comprehensive assessment instrument is intended to replace subjectivity with objectivity and inconsistency with consistency.” Other states and vendors echo similar goals.
States respond to underfunding of HCBS programs by working with vendors to create technical infrastructure to determine eligibility and then claim the eligibility determinations are fair and accurate. In doing so, states constrain the political terrain, pushing advocates toward engaging with state agencies on technical questions about assessments and algorithms.
In this report, we identify four mechanisms that are crucial for advocates to understand in order to see how state agencies obscure and depoliticize eligibility determinations:
Focusing on accuracy: State agencies claim that their automated determinations can identify the “right people” — i.e., those who “should” be eligible for HCBS programs. In reality, LOC algorithm design yields politically tolerable rates of eligibility denials, while still denying care to people who need it.
Deferring to vendors: Standardized assessments and vendors’ recommendations heavily influence state rulemaking and algorithm design. States justify their eligibility determinations by pointing to vendor decisions, invoking the validity and reliability of the vendors’ assessments. Vendor choices about how to phrase and score questions result in LOC algorithms that alter and often narrow states’ regulatory definitions of the institutional level of care.
De-emphasizing the role of LOC algorithms: In public materials, state agencies focus discussion on the selection and administration of the standardized assessment and rarely discuss the extensive and subjective process of developing the algorithm that actually determines eligibility using the assessment as input.
Concealing assessments and algorithms: State agencies rarely make the standardized assessment and accompanying materials, such as user manuals, publicly available and almost never make the algorithm available, invoking vendors’ proprietary interests to protect this information from scrutiny — even in the face of due process claims and, in some cases, court orders.
In this section, we explore these four mechanisms in practice through case studies in Washington, DC, Missouri, and Nebraska. We focus on these three jurisdictions because we were able to obtain more substantial information about their algorithm implementation process. We hope that advocates will do this exercise for their own states. We provide some tips on doing so in the Advocacy Tools section of this report and encourage advocates interested in analyzing their states’ LOC algorithms to reach out to us for support.
Case studies
The following case studies draw on documents we obtained through our public records requests, as well as documents released by state agencies, to provide a view into the design and implementation of LOC algorithms. Looking at rulemaking to refine the institutional level of care in Washington, DC, for example, reveals the interRAI HC assessment’s heavy influence on the regulations and the local Medicaid agency’s resistance to making the assessment available to people who are denied eligibility.
Meanwhile, the Missouri case study shows how mapping the state LOC regulations to the LOC algorithm narrowed who is deemed eligible for home and community-based services. This contrasts with Missouri’s nursing facility eligibility, which is more inclusive despite relying on the same regulations. In contrast to most states, Missouri published draft and final versions of its LOC algorithm on the state agency website. The state agency’s transparency about the algorithm and development process enabled us to examine the ways in which the state uses the interRAI HC and LOC algorithm to legitimize its eligibility determinations.
Lastly, our case study on Nebraska uses vendor reports and minutes from meetings between the state agency and its vendor to show how the vendor shaped eligibility in the state — highlighting, as one of the consultants is quoted as saying to state agency employees in the meeting minutes, that “the idea of LOC and eligibility being clear cut is a myth.”
Case study: Washington, DC
In July 2018, DC’s Medicaid agency, the Department of Health Care Finance, began using a new process to determine eligibility for all long-term care for elderly people and people with physical disabilities, including institutional care in a nursing facility. DC worked with its vendor FEI Systems Inc. to switch to using interRAI’s HC assessment and developed a new LOC algorithm. Of the 1,591 people whose eligibility was redetermined between July 2018 and April 2019, 14 percent lost access to home and community-based services because they did not meet the new level of care requirement.
Defining DC’s Institutional Level of Care
As part of the switch to the interRAI HC and the new LOC algorithm, the Department of Health Care Finance went through two rulemaking processes to update its eligibility regulations. The first, from November 2016 to July 2017, updated the LOC criteria and scoring. The second, from February 2019 to April 2021, “update[d] the requirements of the Long Term Care Services and Supports assessment process to align with the new standardized needs-based assessment tool [the interRAI HC] utilized by the District.”
The agency deferred significantly to the interRAI HC assessment in its rulemaking process. One example of the influence of the interRAI HC on DC’s regulations is in the definition of the lookback period, or the period of time prior to the assessment that the assessor asks about and that is used to determine people’s needs. For most questions, the interRAI HC uses a lookback period of three days. Prior to the switch to the interRAI HC, DC used a seven-day lookback period.
In their comments on the proposed rule, legal advocates from Disability Rights DC at University Legal Services and Legal Counsel for the Elderly raised concerns that the new lookback period is too short to accurately assess people’s needs. The agency’s response was that “the three (3) day look-back period for the functional assessment is the length required by the standardized assessment tool now utilized by DHCF (interRAI HC) to provide a more precise understanding of an individual’s current care and support needs while reducing the likelihood of recall errors common with longer look-back periods.” The agency went on to argue that if the three days prior to someone’s assessment do not reflect their typical needs, they could request to reschedule their assessment or request a reassessment — actions that add further delays and administrative burden to an already-burdensome process.
Despite this seeming deference to interRAI, the Department of Health Care Finance’s algorithm does not use all of the questions on the interRAI HC assessment. The agency chose not to include the interRAI HC Meal Prep question in its LOC scoring, for example, even though its previous assessment tool did ask about meal preparation needs as part of the question on eating. In the InterRAI HC assessment, Meal Prep is a separate instrumental activity of daily living, distinct from the Eating activity of daily living. The Department of Health Care Finance or its vendor therefore chose to adopt the Eating question from the interRAI assessment but not the Meal Prep question. As a result, DC’s new LOC algorithm no longer considers whether someone needs help with meal preparation, a departure from both DC’s previous assessment and from the interRAI HC assessment. In fact, the agency decided not to include any of the interRAI HC instrumental activities of daily living in the algorithm except for Medication Management.
The agency’s rulemaking process also protected and enshrined interRAI’s proprietary interests. The proposed rule suggested making a copy of the assessment and user manual available for inspection in-person at the agency’s office, which Legal Counsel for the Elderly pointed out would be difficult or impossible for people who are homebound. In their comments on the February 2019 proposed rule, both University Legal Services and Legal Counsel for the Elderly recommended that the Department of Health Care Finance instead make a copy of the assessment and the user manual available on its website. University Legal Services argued that not making the assessment available for review online, as the previous assessment had been, “fail[ed] to constitute legally sufficient notice prior to the denial, reduction, or termination of [Long Term Care Services and Supports].”
The agency’s response to these comments was to state that “the InterRAI Home Care (HC) Assessment System is a proprietary tool with copyright protections that restrict its reproduction or transmittal.” It went on to say that its licensing agreement prohibited the posting of the assessment and user manual online. Meanwhile, the interRAI HC assessment and user manual is available for purchase on interRAI’s website for $71.95.
University Legal Services also recommended that in order to meet due process requirements, the Department of Health Care Finance should provide assessment and scoring reports to anyone who receives a denial, reduction, or termination of benefits. The agency responded, “DHCF does not agree that the inclusion of completed assessment reports and scores is necessary for compliance with the notice and due process requirements described above.”
University Legal Services commented that the LOC algorithm “fails to incorporate dementia into the cognitive/behavioral score.” The agency responded that “instead of looking at whether an individual has been formally diagnosed with dementia, the cognitive/behavioral assessment evaluates the presence and frequency of a variety of behaviors and abilities, many of which correspond to the symptoms of dementia.” The LOC algorithm’s Cognitive Score includes questions from two sections of the interRAI HC: Section D, Communication and Vision, and Section E, Mood and Behavior. In addition to omitting the interRAI HC question on diagnosis of dementia, the algorithm also does not include any questions from Section C, Cognition.
The agency’s responses to advocates’ comments on the proposed eligibility rule demonstrate a deference to the interRAI HC in some areas, such as to justify using a three-day lookback period and denying online access to the assessment. While in other moments, such as to justify not including any Cognition questions from the interRAI HC, DHCF’s responses defer to its own algorithm, designed by a different vendor. The advocates’ comments and the agency’s responses demonstrate the contestable and subjective nature of what is factored into an eligibility determination.
Case study: Missouri
Missouri’s Department of Health and Senior Services is unique in our review because the agency made its LOC algorithm publicly available, both as it was going through revisions and once it was finalized. Missouri’s process of updating its LOC scoring and the algorithm that implements them began in 2017, after the state legislature made multiple changes to Medicaid long-term care with the goal of reducing spending. This included raising the LOC score required to be eligible for home and community-based services from 21 to 24 points.
Defining Missouri’s Institutional Level of Care
With the new higher LOC threshold, the Department of Health and Senior Services was concerned that people were losing eligibility who it did not think should be, so the agency decided to embark on an “LOC Transformation” project to revise the way the LOC score was determined. The stated goal for this project was “to review all aspects of the HCBS assessment process to ensure the right services are provided to the right individuals at the right time.”
In 2017, the agency therefore began a multi-year process of developing and implementing a new LOC algorithm for HCBS eligibility. As part of this process, the Department of Health and Senior Services went through a rulemaking process to update the state’s LOC criteria, which apply to both nursing facilities and home and community-based services. It contracted with Princeton University’s State Health and Value Strategies team and Go Long Consulting to conduct a review of state LOC models, carry out stakeholder engagement sessions with agency staff and nursing facility and home care agencies, and develop the new LOC algorithm. Go Long Consulting developed the new LOC algorithm, proposing the first version in 2018. The state Medicaid agency publicly released the first version of the proposed algorithm in December 2018.
Although Missouri’s choice to publish its proposed algorithm exhibited a high level of transparency, advocates and people using home and community-based services struggled to evaluate the impact of, or identify issues with, the algorithm based on the logic alone. Upturn worked with Legal Services of Eastern Missouri to audit the proposed algorithm using a sample of assessment data and found that it would disqualify as many as 66 percent of currently eligible people.
After our audit, the state contracted with Mercer to audit version 2.2 of the algorithm. Mercer found that 19 percent of then-eligible people would no longer be eligible. The agency further revised the algorithm, and the resulting version 2.3 algorithm was fully implemented in October 2024. The state did not conduct an audit of version 2.3 but estimated that it would cut 8 to 9 percent of currently eligible people.
Figure 5. Mobility question on Missouri’s Nursing Facility Assessment
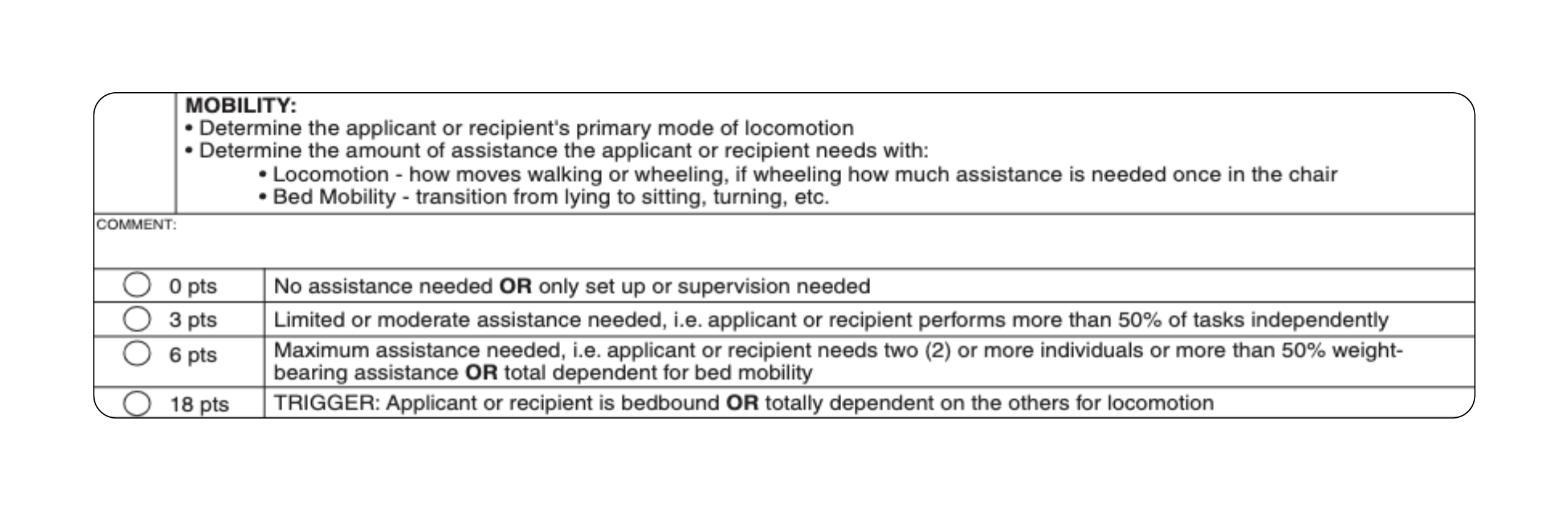
Figure 5. Mobility question on Missouri’s Nursing Facility Assessment. This figure shows the Mobility question on Missouri’s nursing facility assessment. Source: Department of Health and Senior Services, 19 CSR 30-81, Nursing Facility Level of Care Assessment, March 31, 2022, https://www.sos.mo.gov/CMSImages/AdRules/csr/current/19csr/19c30-81a.pdf.
If developing a LOC algorithm to determine who should receive home and community-based services was actually an objective task, then each version of the algorithm Missouri proposed should have found a similar proportion of people eligible and ineligible. Instead, the fact that the first version of the algorithm would have cut off 66 percent of people surprised the state because they did not intend to cut that many people off the program. The Department of Health and Senior Services then tweaked the algorithm seemingly to arrive at a more acceptable percentage of denials.
The updated LOC algorithm seemed to provide a rationale for the agency to implement cuts in a way that the agency found logical and palatable. Through webinars for home care providers, the state agency worked to justify the new algorithm and build buy-in from providers by offering various rationales for why some of their clients might be cut off from needed care services. The rationales included saying that some people might lose their eligibility because they “misrepresented” their situation during the COVID-19 public health emergency, when the assessor wasn’t there face-to-face to observe.
The agency also provided messaging advice for assessors to prepare when going into an assessment where the person is likely to lose eligibility, encouraging them to use their time on the car ride to the person’s home to think about what they would say to explain the person’s ineligibility, seeing it as “our chance to have an excuse.” One webinar also encouraged assessors to document the assessment process and get confirmation from the person being assessed that they understood it so that at a hearing, a person trying to appeal their HCBS denial would not be able to say that they didn’t understand the assessment questions.
Missouri’s eligibility determinations for nursing facilities differ from its determinations for home and community-based services, further highlighting the political nature of these tools. In Missouri, the same LOC regulations apply to both HCBS eligibility and nursing facility eligibility. Under federal law, eligibility for home and community-based services and nursing facilities should be the same. Yet Missouri gives nursing facility assessors much more discretion to determine eligibility under the same regulations. The assessment for nursing facility eligibility shows the possible number of points and descriptions for each question as shown in the screenshot of the Mobility question on Missouri’s nursing facility assessment in Figure 5.
Unlike the regulations and the nursing facility assessment, the interRAI HC question for locomotion explicitly excludes assistance needed to go up and down stairs. As such, the use of the interRAI HC as input to the LOC algorithm functionally narrows the criteria set out in the regulations, limiting points people can get for mobility needs. This means someone who needs help going up and down stairs could score higher on the nursing facility eligibility determination than on the LOC algorithm used for home and community-based services.
Other examples of differences between how someone is assessed for nursing facility and home and community-based services eligibility include Balance and Rehabilitative Services. For Balance, the nursing facility assessment tool asks assessors to score people based on “current problems with balance” generally, but to get the same score on the HCBS algorithm, someone would need to have had problems with balance in the past three days.
For the Rehabilitative Services category, the regulations require an evaluation of a person’s need for and receipt of physical therapy, occupational therapy, speech therapy, or cardiac therapy services. The HCBS LOC algorithm differs from the state regulations and the nursing facility tool because it assigns points based on how many times someone received a service in the past seven days, whereas the regulations and nursing facility tool assign points based on how many times a week the person is supposed to get services. So, if someone is supposed to receive rehabilitation services every week but did not in the week prior to their assessment for whatever reason, they may get 0 points for this section in the HCBS LOC algorithm but would get 3 points in the nursing facility tool.
The discrepancies between the number of people made ineligible in each version of Missouri’s LOC algorithm and the differences in eligibility determinations between home and community-based services and nursing facility assessments demonstrate the subjective nature of the determinations that are allegedly identifying the “right people” to get home and community-based services.
Case study: Nebraska
In 2020, Nebraska’s Department of Health and Human Services’ Division of Developmental Disabilities took on the administration of the state’s Aged and Disabled waiver. The division contracted with Optumas, a health care consultancy based in Arizona, to evaluate and recommend options for an assessment tool and an LOC algorithm.
Defining Nebraska’s Institutional Level of Care
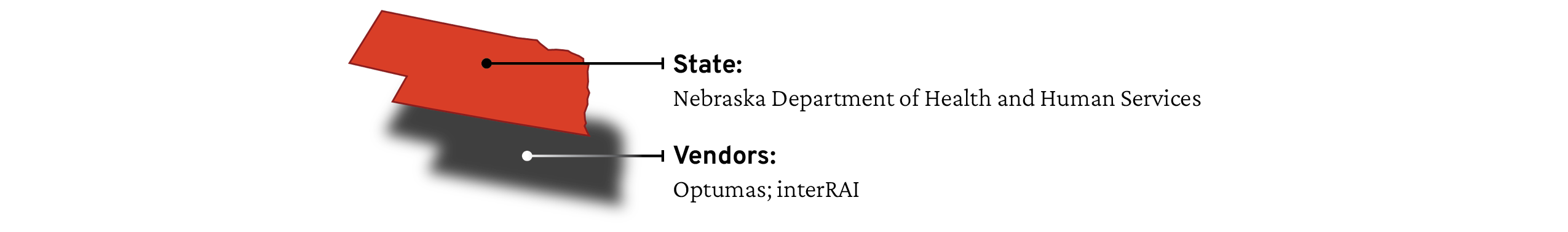
In a June 2020 report, Optumas recommended the Division of Developmental Disabilities replace its existing assessment with the interRAI HC. One of the reasons Optumas gave for the switch was that the interRAI HC covers more domains, including instrumental activities of daily living, which were not present on Nebraska’s assessment in use at the time. Following these recommendations, the division worked with Optumas to implement the interRAI HC assessment and to develop and test a scoring algorithm to determine institutional level of care using the interRAI HC as input. It began using the interRAI HC and new LOC algorithm in July 2021.
As part of the implementation of the interRAI HC and new LOC algorithm, Optumas recommended Nebraska make slight changes to the criteria in the regulations to more closely align with the interRAI HC. For example, Nebraska’s regulations previously defined Bathing as “The ability to get to the bathing area and cleanse all parts of the body and the hair to maintain proper hygiene and prevent body odor, including tub, shower, and/or sponge bath.” Yet the interRAI HC definition of the Bathing activity of daily living explicitly excludes washing one’s hair and back. The revised Nebraska regulations removed the mention of hair in the definition for Bathing. Even after the revisions, the regulations still state “bathing each part of the body,” but the LOC algorithm uses the interRAI HC Bathing question. As such, someone who is able to bathe without support but is unable to wash their back would score as not needing assistance on the Bathing question. While amending state regulations requires a public process involving notice and opportunities for comment, implementing regulations in the form of a LOC algorithm involves significant discretion yet isn’t subject to a public process.
Prior to working with Optumas, Nebraska’s regulations already had a fairly comprehensive view of what should be considered for institutional level of care through three risk factors: Behavior, Frailty, and Safety. Optumas also took an expansive view in its recommendations for how to map these regulatory definitions to the interRAI HC, including interRAI HC questions on housing and the availability and willingness of informal caregivers to continue providing care. Nebraska’s is the only LOC algorithm we analyzed that incorporates interRAI HC questions on decline in social activities, reliance on informal help, and housing. Nebraska’s algorithm also uses the largest number of instrumental activities of daily living, including managing finances, shopping, and phone use.
Notably, in its redesign project, the state directed Optumas to minimize the impact of the new assessment and eligibility algorithm, meaning that the goal was not to reduce the number of people qualifying for the Aged and Disabled waiver. Analysis of the new algorithm also showed that Nebraska had a higher eligibility rate when compared to five other states, something the vendor sought to confirm Nebraska actually wanted. In meeting minutes we obtained through our public records request, the contractors were documented as telling Nebraska’s Division of Developmental Disabilities that “it is up to you whether or not you want to tighten it up and whether that is feasible,” pointing out that making people eligible based on needing supervision on activities of daily living “is not typical” but that a lot of differences across states are “due to policy characteristics.” The contractors also said, according to meeting minutes, “. . . there are some states that adjust their LOC regulations to accommodate changes in budget. Which could also explain the lower rates,” meaning that budget reductions could explain the lower rates of HCBS eligibility in other states.
Nebraska took a relatively expansive approach to eligibility. The meeting minutes show one agency employee responding to the inquiry from the vendors about adjusting the LOC algorithm to lower the eligibility rate by saying, “I am more concerned about someone not being found eligible that should have been than I am about cases that fall in the opposite direction. Even if Nebraska has the highest, I believe that this aligns with our values.”
This visibility into Nebraska’s LOC algorithm development process illustrates that changes to eligibility, changes that impact the daily lives of clients seeking government services, are ultimately a reflection of policy choices — choices made behind closed doors, in collaboration with private entities. The idea that LOC algorithms are fair and objective tools that accurately measure an individual’s needs and, in turn, can accurately determine eligibility, is a narrative myth upheld by technology. LOC algorithms are actually one of many ways that state agencies can control the size of their eligible population based on budget constraints and policy considerations about who they want to include and exclude, given limited budgets. As meeting minutes from Nebraska’s implementation process say, “the idea of LOC and eligibility being clear cut is a myth.”
While tweaking an algorithm is a critical way to reduce harm by expanding eligibility as much as possible, it will never, by definition, resolve the political problem at the heart of HCBS, which is the need to restrictively define eligibility in order to minimize access to services.
V. Advocacy tools
Our political climate presents a difficult terrain for fighting for universal care, but there are still many tools that advocates can use to help get people the care they need while building toward fights for broader changes to our health care system. Advocates can challenge the depoliticization of eligibility determinations by countering narratives of “accuracy” and “objectivity,” exposing vendors’ influence, and bringing algorithms to light.
This section begins with a brief overview of the current political landscape, then provides practical recommendations for challenging eligibility determinations. When advocates challenge state decisions about LOC algorithms, they can bring these decisions back into the political arena where they belong. Recommendations include ways to learn more about your state’s LOC algorithm, understand the impact of the algorithm, and mount collective challenges against it.
What advocates are up against
People with disabilities and people on Medicaid are facing an all-out assault on their rights and access to benefits. In July 2025, Congress passed sweeping cuts that will severely constrain HCBS budgets and make it difficult for millions of people to survive. The Trump administration’s attack on Medicaid is a massive escalation of a longstanding policy of cuts and service reductions that advocates and organizers have been creatively trying to mitigate for decades. Even the expansion of Home and Community-Based Services itself initially occurred at a time of broader budget cuts under the Reagan administration.
Millions of people’s lives were improved through the expansion of the program, even if limited eligibility and budget constraints were built into the program from the start by the federal government. The lesson here is that advocates and organizers can still extract concessions and build up small wins under difficult political circumstances. But the limitations of these wins, along with the federal government’s obsession with tying home and community-based services to lower costs of long-term care, throw into sharp relief the necessity for universal care.
While faced with many constraints, advocates can continue to push for reforms that expand access to care. Using these efforts to expose the injustices of the HCBS determination process can help build power and make the case for universal care. In 2023, for example, Rep. Debbie Dingell (D-MI), former Sen. Bob Casey (D-PA), and former Rep. Jamaal Bowman (D-NY) introduced the HCBS Access Act, which would have made Home and Community-Based Services an entitlement under Medicaid, meaning states have to provide home and community-based services to anyone who meets the eligibility requirements. It also would have effectively eliminated the institutional level of care by saying that anyone who is eligible for Medicaid and whose provider determines that they have a functional impairment can get home and community-based services. While the bill did not pass, it laid out a vision for reforms that would move us closer to universal home care.
Where does work on LOC algorithms fit within this political landscape? At Upturn, our work navigates how political questions are often obscured as technical questions. Advocates often find themselves in the position of trying to evaluate whether a LOC algorithm is “good” or how they can fix it to make it more fair. Yet the technocratic narratives around HCBS determinations and the atomized nature of the appeals process constrain the questions advocates can ask and the demands they can make.
While tweaking an algorithm is a critical way to reduce harm by expanding eligibility as much as possible, it will never, by definition, resolve the political problem at the heart of HCBS, which is the need to restrictively define eligibility in order to minimize access to services. As such, advocates should approach efforts to tweak algorithms carefully: By narrowly focusing on technical questions, advocates may miss the forest for the trees. Instead, approaching these problems as political questions can connect them to broader political fights for universal care.
This report aims to help advocates, people going through HCBS determinations, and others understand how states define the institutional level of care and enforce it through LOC algorithms. Through this report and our ongoing technical assistance work, we aim to support challenges to automated eligibility determinations that reduce the harms of LOC algorithms with the understanding that it is not possible to develop a LOC algorithm that is fair and accurate (if, by fair and accurate, we mean providing critical services to people who need them). Just as states work with vendors to accomplish their policy goals using LOC scoring, we want to encourage and equip advocates to engage with eligibility determinations as political tools to accomplish their policy goals.
By understanding LOC algorithms as one tool among many that states use to reduce spending, we aim to move the debate beyond narrow technical disputes about the design of LOC algorithms to broader, collective fights about expanding budgets for and access to home and community-based services. Ultimately, our vision is universal access to long-term care in people’s communities. Just as there was a move away from institutionalization and toward care in home and in community, we argue for a move away from the institutional level of care requirement and toward universal access.
Below, we provide practical tools and questions that advocates can use to access, analyze, and challenge their states’ LOC algorithms.
Getting information about your state’s LOC algorithm
Concealing assessments and algorithms is one of the main mechanisms used by state agencies and vendors to depoliticize LOC algorithms. Trying to access these materials is a useful place to start.
LOC algorithms are difficult to obtain because the private vendors that make them often use proprietary claims to keep them inaccessible. Yet even in the rare case when a LOC algorithm is made public, as in Missouri, it may be difficult for people to understand or analyze its real world impact.
Even still, it is possible to gain a better understanding of how a state is determining eligibility using the level of care. If you are not already familiar with your state’s regulations on the level of care, you can start by reviewing those to see how much the criteria and scoring are spelled out. You can also review your state’s waiver applications to see if any additional details that are not in the regulations are included there.
Figure 6. Pseudocode for Activities of Daily Living in Nebraska’s LOC Algorithm
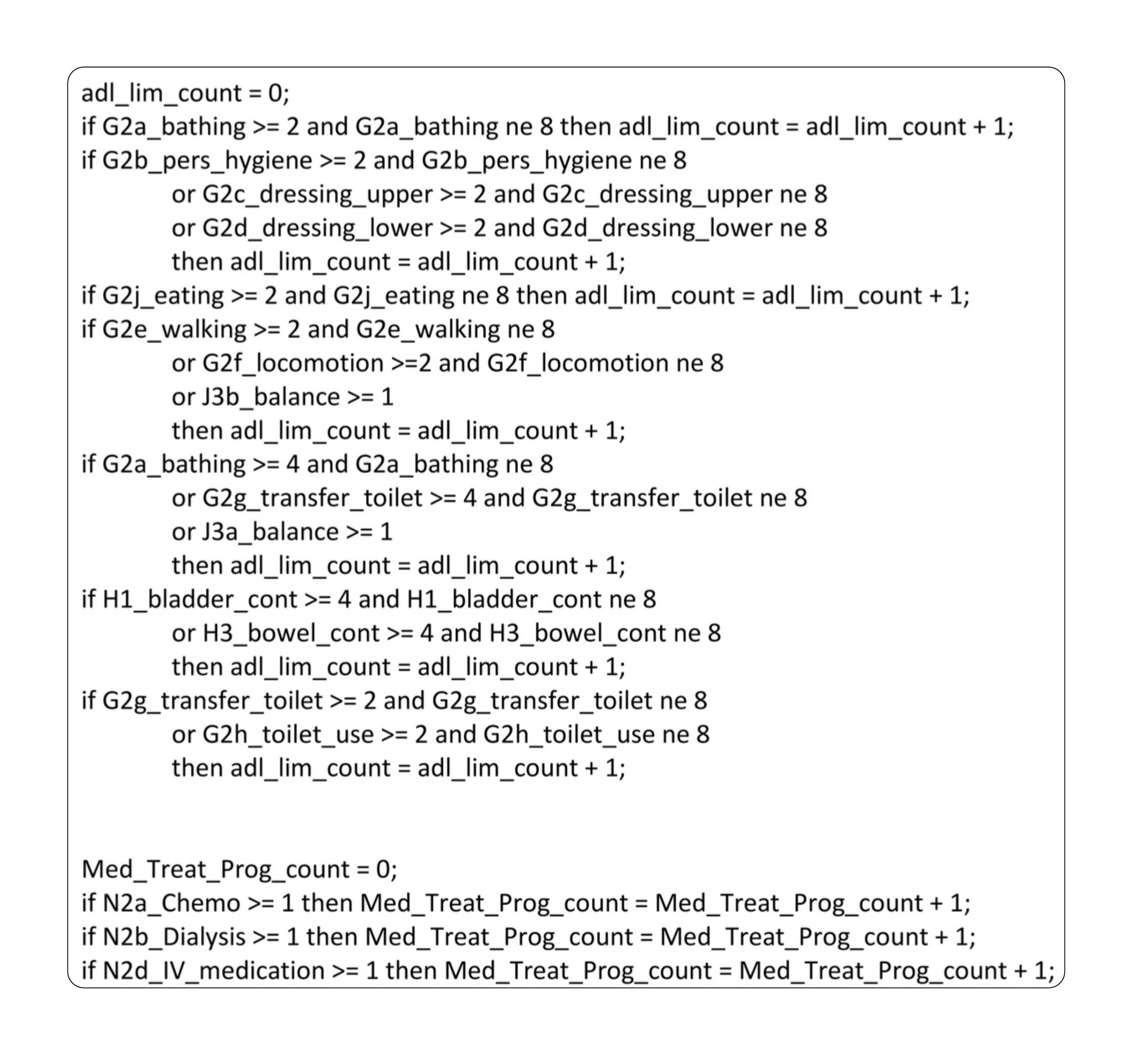
Figure 6. Pseudocode for Activities of Daily Living in Nebraska’s LOC Algorithm. Source: obtained through public records request, https://www.documentcloud.org/documents/26053849-ne-hcbs-adult-assessment-implementation-support-20211025-final-to-state/, pg. 48.
Another potential avenue to learn more about the LOC criteria is through your state legislature’s oversight of the state Medicaid agency. For example, in Washington, DC, the Medicaid agency provided details on its new LOC algorithm in its oversight report to the DC Council. Vendor reports, sometimes available online, are another place where you might be able to obtain some information about the algorithm. You also may be able to find information on vendor websites about their process for designing LOC algorithms.
The next step is more challenging but will enable a much more robust understanding of the LOC algorithm: getting access to the algorithm’s logic. This logic could take the form of pseudocode (see an example from Nebraska in Figure 6), a spreadsheet, or a series of if/then statements. Whatever the format, it is important that the logic include the specific assessment questions that are factored into the LOC score and how each possible score or pathway can be reached. In addition, you will need access to a copy of the assessment that is used as input to the algorithm and an explanation of how to score the assessment questions.
The logic alone does not provide all the information needed to understand the political choices that inform algorithms. States and vendors often have internal analyses that are used to decide where to set cut-offs and tweak the algorithms and assessments accordingly. These can give insight into the motivations of state agencies but are difficult to obtain.
If your state has not made the LOC algorithm logic publicly available, there are several ways you can try to gain access to it:
Submit a public records request (see our public records template in the appendix and the public records request guide from the Benefits Tech Advocacy Hub). Anyone can submit a public records request to their state.
Put pressure on your state Medicaid agency to share the algorithm logic, especially if it is going through a publicized redesign project or applying for or renewing a waiver. If your state is in the process of selecting a contractor or assessment, you can push for disclosure of the logic to be included in the contract. You can point to Missouri as an example and emphasize that providing the algorithm logic builds trust and collaboration between the agency and the people affected by it. You can point out that sharing the algorithm is also in the best interest of the state agency, as it can give advance notice to the state of problems in their algorithm that might not be intended.
If you are a legal advocate or someone appealing your own HCBS determination, you can try requesting the algorithm logic through the appeals process. It may be provided to you in writing before the administrative hearing. At the hearing, you also can ask questions of the state’s witnesses about how the algorithm works. Failure to provide the algorithm denies due process by failing to explain the reasons for the denial or termination of benefits.
If you are suing the state as a legal advocate or person who was denied or cut from home and community-based services, you can request the algorithm logic through discovery. If your state has been sued, you may be able to get access to the algorithm logic through the case filings by contacting the lawyers who brought the suit and/or checking the state legal department website (or searching the internet for the case name).
Work with allied legislators and ask them to request the information and data from the agency.
Organize people receiving or trying to access home and community-based services to testify in front of your state legislature about the importance of access to the algorithm and their due process rights.
Reach out to a host of legal aid organizations, legal aid clinics, state protection and advocacy organizations, pro bono programs, and self-advocacy organizations as potential sources of assistance. The Center for Democracy and Technology’s 2020 report on benefits determinations has a helpful list.
Gaining more information about the LOC algorithm can be a good starting point for collaboration among legal and community organizations. If you are a legal advocate and you are able to gain more information about how your state’s LOC algorithm works, consider working with a community organization to create a short explainer or other materials that can be used to support outreach and training.
Analyzing your state’s LOC algorithm
If you are able to get access to the LOC algorithm, analyzing it collectively with people bringing different forms of expertise — legal, community organizing, policy, and lived experience — is a great way to deepen your shared understanding of how the algorithm works and how it is impacting people. This is also a way to fight back against the state’s attempt to de-emphasize the role of LOC algorithms, which is one of the mechanisms states use to depoliticize the determinations process.
Having a better understanding of your state’s LOC algorithm is a means to an end. It is a tool you can use for various types of advocacy, litigation, and community organizing in order to demand changes to LOC algorithms, including being treated as a political question and not a technical one left to experts. You can also use this analysis to try to understand why a pattern of denials or terminations is occurring, for example, if people who have balance issues and are at risk of falling are not being determined eligible.
Even if there is not an active issue with the LOC algorithm in your state, people who are receiving or applying for home and community-based services can benefit from understanding how the state determines institutional level of care. Learning about the institutional level of care together can be a way for people to build relationships, support each other with their determinations and appeal processes, and identify issues to organize around. It also challenges the narrative of state agencies that tends to defer to vendors and focus on accuracy.
The federal government hands states a broad eligibility standard with the institutional level of care. The process of defining institutional level of care at the state level and implementing an algorithm to enforce it involves a series of choices about what needs to be prioritized and how to measure those needs. While who should be eligible for home and community-based services is an inherently political question, it is transmuted into a measurement question through this process. Analyzing your state’s LOC algorithm is therefore both a way to do basic fact-finding about the LOC algorithm and its impacts and a way to develop a counternarrative that highlights the political nature of the determinations.
Below are some questions to get you started with understanding your state’s LOC algorithm and what it reveals about the state agencies’ and vendors’ definition of the nursing facility level of care.
Agency and vendors:
Who is the standardized assessment vendor?
Who is the implementation vendor?
Who is the consulting vendor?
How do the agency and vendors talk about the eligibility determinations? What rationale do they seem to be using to legitimize them?
Does the agency talk about who they are trying to serve or prioritize?
Was there a budget or legislative change that precipitated a redesign of the eligibility determination process?
Does the agency rely on the claims we have discussed in this report? This includes serving the “right people,” consistency, fairness, accuracy, and objectivity.
Regulations:
How much is the level of care defined in your state’s regulations? Do the regulations list out specific pathways or numbers of points that people can get in different categories?
What do the regulations reveal about what the state agencies are prioritizing? For example, do the regulations talk about safety or well-being? Do they include instrumental activities of daily living? Do they give people points for needing minimal support or supervision, or only for extensive support needs?
What differences can you find between the regulations and the algorithm? How does the LOC algorithm change eligibility as defined in the regulations?
For specific questions, are there more exclusions or details in the assessment than what is present in the regulations? For example, the interRAI HC does not consider support needed for washing one’s hair and back in the Bathing activity of daily living, but the regulations may not specifically exclude this.
How does the nursing facility eligibility assessment work? Does it more closely adhere to the regulations?
If you are trying to address a specific issue, does it seem like it arises from the regulations themselves or from how the regulations are implemented in the algorithm? For example, if people who are at risk of falling are not being determined eligible, do the regulations explicitly talk about whether risk of falling is part of the LOC criteria or not?
Algorithm design:
What assessment is being used as input to the algorithm? Are there any other inputs?
Does the LOC algorithm use an accumulation scoring approach or a pathways scoring approach?
If accumulation, how many points are required to meet the institutional level of care?
If pathways, what are the possible pathways to meet the institutional level of care?
What does the algorithm reveal about what the state agencies and vendors are prioritizing?
Which questions from the assessment are considered in the LOC algorithm?
What categories or sections of questions are included?
Which possible ratings on those assessment questions increase someone’s score? In other words, how much support does someone have to need in order to score points on the algorithm? For example, do people get points for needing supervision and cueing on activities of daily living and instrumental activities of daily living or only if they need hands-on support?
How are different questions and ratings weighted? For example, a question might be included in the algorithm but contribute relatively few points or only count in a pathways algorithm if other conditions are met first. Or, for example, needing support with eating might get you more points than needing support with bathing.
Understanding the impact of the algorithm:
Are you noticing a pattern of people losing eligibility?
Can you reach out to community organizations that work with elderly people and/or people with disabilities to find out who is being cut?
Can you reach out to organizations that can test the algorithm against a dataset from your state to see what the impact would be? This can include reaching out to the Benefits Tech Advocacy Hub.
What factors do other states’ algorithms consider that are or are not considered in your state? Consider differences across states in budgets, eligibility rates, and available services in this comparison.
How much discretion do other states’ regulations provide for their algorithms?
Challenging your state’s LOC algorithm
Since LOC algorithms are designed to target HCBS eligibility to some people and not others, you will likely find that there are specific issues with your state’s LOC algorithm that arise from the algorithm not considering or prioritizing certain needs or other important factors. While changes to the algorithm will not address the underlying lack of funding, they can reduce the burden of harm-reduction fights on that particular issue.
State agencies like to pretend that LOC algorithms are accurate and valid. Publicizing challenges to the algorithm can help shatter this illusion. We are also interested in whether efforts to make changes to the algorithm can be an entry point to organizing that can build toward bigger fights, including campaigns to increase the budget for home and community-based services or significantly expand eligibility.
Through our technical assistance work, we have seen some of the limitations of challenges to automated benefits determinations. Typically challenges to eligibility determinations are limited to individual appeals, which are burdensome. Even if someone wins their appeal, the state is not required to fix the issue for anyone else. As a result, legal services providers have filed numerous lawsuits after recognizing patterns of cuts and terminations across their clients and identifying systemic issues with their state’s HCBS determinations. However, these legal challenges are often limited by legal services’ funding constraints.
In some states, advocates have also engaged proactively with their state Medicaid agency when the agency is making changes to its assessments and eligibility criteria. We see challenges focused on making changes to the algorithm to reduce its harms as important and as more useful the more they involve building relationships and shared understanding of the algorithm and its impacts across legal and community organizations and the people immediately affected by HCBS funding.
Here are a few tactics you can use to draw attention to the issues with your state’s LOC algorithm, bring people in, and develop demands for changes to how your state determines eligibility for home and community-based services:
Client stories: You can collaborate with people who need home and community-based services but were not found eligible and share their stories, making a case for why the LOC algorithm should consider their needs and fails to. A 2020 report from the Center for Democracy and Technology mentions a number of tactics for storytelling, including town halls, hearings, and listening sessions; social media; op-eds, letters to the editor, and outreach to journalists; and outreach to legislators.
Public participation: You can make the most of opportunities when state agencies are required to open up legislative changes for public comment. These can be used as an opportunity to organize people impacted by these changes and provide feedback that can be impactful. For more tips on public participation, see the Benefits Tech Advocacy Hub Public Participation Advocacy Guide at https://www.btah.org/resources/public-participation-advocacy-guide.html.
Community building: Formally participating in public comments is not the only way to make change or participate in policymaking. You also can contact elected officials and state agency officials, and use the complaint process of state agencies to make demands. The more people you can bring together in a unified way in this process, the more effective it might be. Building community, whether formally or informally, and partnering with organizers and community organizations is a major way to get people situated to make bigger demands. For more tips on community building, see the Benefits Tech Advocacy Hub Community Building Advocacy Guide at https://www.btah.org/resources/community-building-advocacy-guide.html.
Media advocacy: Advocates can use storytelling through press and other media to raise public awareness, increase pressure on government officials, and connect more affected people to each other. For more tips on media advocacy, see the Benefits Tech Advocacy Hub Media Advocacy Guide at https://www.btah.org/resources/media-advocacy-guide.html.
VI. Conclusion
The institutional level of care requirement is not designed to meet people’s needs. Rather, it is designed to make long-term care cheaper for the government by reducing people’s access to it. In order for everyone who needs care, whether due to age or disability, to receive it in their homes and communities, we need a universal health care system that includes home care.
Instead of a health care system that makes home care available to people based on their needs, we have a system that puts the majority of home care services behind the barrier of the institutional level of care as defined and operationalized by state Medicaid agencies and a network of private vendors. Not only is the institutional level of care a barrier to people receiving care, but the infrastructure of the level of care also creates obstacles to advocacy by obscuring the political question of who deserves care behind the technical questions of how to accurately identify who should be eligible. The path to actually meeting people’s needs is not making minor tweaks to LOC algorithms but rather building power to fight for the policy and funding changes that would make home care available to everyone who needs it.
People trying to access home and community-based services and their advocates are already fighting unjust determinations. We are grateful to people who have educated us about what is happening on the ground. These are important harm-reduction fights that can get people immediate access to care that helps them safely live at home. With our work on LOC algorithms, we want to support efforts to get people access to the care to which they are entitled under current policies while also building connections that will help us make bigger demands. In the nearer term, that could look like pushing for increased funding for home and community-based services or making more services available as part of the Medicaid state plan so that states can’t deny these services to people using LOC algorithms or waitlists.
The institutional level of care is subjective. States and vendors know this and make decisions about how to define the level of care based on their priorities and budgets. We believe that challenging LOC algorithms with this in mind makes it more possible to build toward the broader fights that are needed to actually get home and community-based services to more people who need it. How you challenge the LOC algorithms is also important. The system is set up to rely on individual challenges, but through organizing and litigation, it is possible to pursue more collective challenges that can help build a base of people to mobilize on budget fights in the future and ultimately to fight for universal home care.
Acknowledgements
This work would not be possible without the tireless work of our colleagues and partners. We are grateful to them, and we take responsibility for any errors that remain here. Special thanks to Kevin De Liban, Elizabeth Edwards, and David Machledt for introducing us to this topic and generously sharing their expertise with us. Thanks to People’s Action Institute for inspiring us with their Care Over Cost campaign. We would also like to thank our colleague at Upturn, Ming Hsu, for his contributions to this report.
For their helpful input and feedback on this report, we’d like to thank the following individuals: Henry Claypool, American Association of People with Disabilities; Jaimie Worker and Nicole Jorwic, Caring Across Generations; Ridhi Shetty, Center for Democracy & Technology; Mike Oxford, Disability Policy Consultant; Laura Bernas, Grassroots Disability Advocate; Kate Brady, HSRI Grassroots Project; Hagar Dickman and Natalie Kean, Justice in Aging; Jamie Rodriguez and Joel Ferber, Legal Services of Eastern Missouri; Ian Moura, the Lurie Institute for Disability Policy, Brandeis University; Edison McDonald, National Disability Action; Elizabeth Edwards, Jennifer Lav, and David Machledt, National Health Law Program; Dom Kelly and Kiana Jackson, New Disabled South; Kevin De Liban, TechTonic Justice; Peter Stephan, formerly University Legal Services, Disability Rights DC; Ritchie Eppink, Wrest Collective; and Natasha Duarte, Mitra Ebadolahi, Ming Hsu, Logan Koepke, Tiffany Wong, and Harlan Yu, Upturn. All affiliations are for identification purposes only.
For legal support, we’d also like to thank Jack I. Lerner, UC Irvine School of Law (institution listed for affiliation purposes only) and Kendra Albert of Albert Sellars LLP.
Thanks to Chris Wong and Objectively for assisting with the design of our report and Emilie Openchowski for copyediting.
Upturn is supported by the Democracy Fund, the Ford Foundation, the Heising-Simons Foundation, the John D. and Catherine T. MacArthur Foundation, and Mission Telecom.
Appendix A: Public records requests documents received, by state
Some documents that we obtained via public records requests are not available online. If you work on these issues and would like to review them, please reach out to us at hello@upturn.org.
Public records requests documents received, by state
| State | Documents received, and link to documents |
|---|---|
| California | LOC criteria; HCBS manual https://www.documentcloud.org/projects/222336-california/ |
| Colorado | Billing manual; Colorado regulations; HCBS rates; support-level calculation sheets; SIS respondent guide; support-level definitions; SIS manual appendices; SIS training documents https://www.documentcloud.org/projects/222337-colorado/ |
| Connecticut | Universal assessment; LOC crosswalks; ABI waiver LOC tables; CHCPE waiver LOC tables; HCBS budget tiers; training materials https://www.documentcloud.org/projects/222338-loc-algorithms-report-connecticut/ |
| Florida | Assessment forms; Florida statutes; Florida managed care coverage policy https://www.documentcloud.org/projects/222339-loc-algorithms-report-florida/ |
| Georgia | Policies and procedures manual for home health services https://www.documentcloud.org/projects/222340-loc-algorithms-report-georgia/ |
| Indiana | Aged and Disabled waiver eligibility screen https://www.documentcloud.org/projects/222341-loc-algorithms-report-indiana/ |
| Iowa | Iowa statutes; contract cost; RFP proposals (redacted); training manuals; AIDD agreement; assessment; cost neutrality workbook; assessment manuals; CDAC agreement; LTSS waiver assessment process; internal assessment training documents; Iowa administrative codes; intermediate care facility/intellectual disability level of care criteria; nursing facility level of care criteria; skilled level of care criteria; scoring matrix for rates placement https://www.documentcloud.org/projects/222342-loc-algorithms-report-iowa/ |
| Kentucky | AAIDD quote; training manuals; LOC form; SIS provider letter https://www.documentcloud.org/projects/222343-loc-algorithms-report-kentucky/ |
| Louisiana | Assessment; ADL coding and scoring; RUG/HC descriptions and categories; Louisiana codes; long term-personal care service hours determination guide; NF LOC pathways; service hour allocation guide; nursing facility level of care eligibility manual; assessment guides https://www.documentcloud.org/projects/222344-loc-algorithms-report-louisiana/ |
| Maine | AAIDD contract; AIDD monthly invoices https://www.documentcloud.org/projects/222345-loc-algorithms-report-maine/ |
| Massachusetts | AAIDD RPF response; contract (redacted); AIDD invoices https://www.documentcloud.org/projects/222346-loc-algorithms-report-massachusetts/ |
| Michigan | Assessment; iHC crosswalk (partial scoring logic); LOC criteria; Medicaid provider manual; interRAI assessment manual [available by request] https://www.documentcloud.org/projects/222347-loc-algorithms-report-michigan/ |
| Mississippi | LTSS MS core standardized assessment and level of care functional requirements https://www.documentcloud.org/projects/222348-loc-algorithms-report-mississippi/ |
| Nebraska | Assessment [available by request]; LOC scoring logic; interRAI training documents; ADL descriptions; LOC criteria; HCBS redesign project documents; interRAI scales https://www.documentcloud.org/projects/222349-loc-algorithms-report-nebraska/ |
| New Jersey | ADL/LOC coding; waiver eligibility criteria; algorithm; level of care and assessment process https://www.documentcloud.org/projects/222350-loc-algorithms-report-new-jersey/ |
| New Mexico | Individual service plan document; LTC assessment; Vineland training documents [available by request]; Vineland assessment [available by request] https://www.documentcloud.org/projects/222351-loc-algorithms-report-new-mexico/ |
| Rhode Island | AAIDD purchase order; AAIDD contract; training and information documents; waiver budget tiers; SIS respondent guide https://www.documentcloud.org/projects/222352-loc-algorithms-report-rhode-island/ |
| South Carolina | Assessment; assessment hours guide; assessment procedure manual and training guides; LOC procedure manual; case management procedure manual; service plan procedure manual https://www.documentcloud.org/projects/222353-loc-algorithms-report-south-carolina/ |
| South Dakota | Eligibility criteria; care plan explanation; RUG score chart; waiver policies; provider policies https://www.documentcloud.org/projects/222354-loc-algorithms-report-south-dakota/ |
| Utah | Needs assessment questionnaire tool; LOC determination; training guides; MDS-HC assessment [available by request] https://www.documentcloud.org/projects/222355-loc-algorithms-report-utah/ |
| Washington | SIS training guide; AAIDD contract https://www.documentcloud.org/projects/222356-loc-algorithms-report-washington/ |
| West Virginia | Budget and score sheet; budget methodology; training guide; West Virginia codes https://www.documentcloud.org/projects/222357-loc-algorithms-report-west-virginia/ |
| Wyoming | Budget and scoring methodology; budget amounts; ICAP contract; waiver rates and services index; LT101 assessment; individualized care plan guide https://www.documentcloud.org/projects/222358-loc-algorithms-report-wyoming/ |
Appendix B: Public records requests denials
This table includes states that denied part of our requests even if they provided some documents listed in the table in Appendix A.
Public records requests denials, by state
| State | Reason for denial |
|---|---|
| Alabama | Out of state request |
| Alaska | No response |
| Arkansas | Out of state request |
| Delaware | Out of state request |
| Georgia | Proprietary information |
| Hawaii | No response |
| Idaho | No response |
| Illinois | No responsive records |
| Kansas | Documents publicly available |
| Minnesota | Fee waiver denial |
| Missouri | No responsive records |
| Nevada | No responsive records |
| New Hampshire | No response |
| New York | Proprietary information |
| North Carolina | No response |
| North Dakota | Fee waiver denial |
| Ohio | No response |
| Oklahoma | No response |
| Oregon | Fee waiver denial |
| Pennsylvania | Proprietary information |
| Rhode Island | Proprietary information |
| Tennessee | Out of state request |
| Texas | Fee waiver denial |
| Vermont | Fee waiver denial |
| Virginia | No responsive records |
Appendix C: Public records request template
[DATE]
[ADDRESS]
Re.: Public Records Request — Standardized Assessment Tools
Dear Public Records Officer:
[ORGANIZATION NAME] is conducting a survey of states’ use of the various standardized assessment tools used for Medicaid Home and Community-Based Services (HCBS). This is part of a project [PROJECT DESCRIPTION].
Pursuant to [STATE RECORDS REQUEST LAW AND CITATION], we request the following records pertaining to the standardized assessment tool(s) that [STATE] uses to determine eligibility and service hours or budgets for home and community-based services (HCBS).
We intend this request to cover any automated, semi-automated, or manual processes used to factor the assessment tool(s) into HCBS determinations. For purposes of this request, “HCBS determinations” refers to eligibility for HCBS programs and services, as well as service allocation, including the number of hours, budgets, or other units of service and types of services.
Records Requested
Please provide copies of the following records:
A copy of [STATE]’s assessment tool(s) used for HCBS determinations
Documentation of the logic — such as decision trees, spreadsheets, code, tables, instructions, algorithms, determination guides — used to determine HCBS eligibility
Documentation of the logic — such as decision trees, spreadsheets, code, tables, time-and-task tools, case-mix ratios — used to calculate service needs, including the number of hours, service units, or the budget amount authorized for HCBS services for an HCBS applicant or recipient
Documentation of any other ways [STATE]’s assessment tool(s), in whole or in part, are factored into determinations of eligibility for HCBS or into determining the budget, number of hours, or other units of HCBS service, for which an HCBS applicant or recipient is authorized
Any training materials, manuals, policies, procedures, and practices the agency and any of its contractors follow for using [STATE]’s assessment tool(s) responses in HCBS determinations
Other logic or scoring used as part of HCBS determinations, such as but not limited to time-and-task or service planning tools
Purchasing and procurement documents, including but not limited to purchase orders, RFPs, responses to RFPs, invoices, and contracts for [STATE]’s assessment tool(s)
Internal documents, such as presentations and other informational materials, concerning implementation of [STATE]’s assessment tool(s) and their use in HCBS determinations
This request is made on behalf of a not-for-profit organization whose mission is [ORGANIZATION MISSION]. Because of our not-for-profit status and the fact that this request is about a matter in the public interest, we request a fee waiver. If such a waiver is denied, please inform us in advance if the cost to process this request will be greater than $50.
According to [STATE RECORDS REQUEST LAW], a custodian of public records shall comply with a request [WITHIN X BUSINESS DAYS OF RECEIPT / TIMEFRAME SPECIFIED IN THE LAW]. Please furnish all responsive documents to [CONTACT NAME] at [CONTACT INFORMATION] or by mail to:
[ORGANIZATION]
[ADDRESS]
If it would be helpful, we welcome a phone conversation to discuss or refine this request. If you have any questions or want to discuss this request, please contact me by phone at [PHONE NUMBER] or by email at [EMAIL] within the above timeframe. Thank you for your prompt attention to this matter.
Sincerely,
[NAME]
1
Medicaid and CHIP Payment and Access Commission, Federal Requirements and State Options: Eligibility, March 2017 https://www.macpac.gov/wp-content/uploads/2017/03/Federal-Requirements-and-State-Options-Eligibility.pdf (table detailing eligibility requirements at the federal level, as well as options for states to extend coverage).
1
KFF, Number of Dual Eligible Individuals, 2025, https://www.kff.org/other/state-indicator/number-of-dual-eligible-individuals/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
1
Additional HCBS waivers are approved through Section 1115 of the Social Security Act. These are called demonstration waivers and are more flexible. States use demonstration waivers for HCBS programs that involve self-directed services enabling people to hire their own care workers, including to pay family members and friends for their care work. In 2024, 14 states were using 1115 demonstration waivers for home and community-based services, serving more than 1.1 million people. See Maiss Mohamed, Alice Burns, et al., What is Medicaid Home Care (HCBS)?, Kaiser Family Foundation, February 18, 2025, https://www.kff.org/medicaid/issue-brief/what-is-medicaid-home-care-hcbs/.
1
42 U.S.C. § 1396n (c)(3) (“A waiver granted under this subsection may include a waiver of the requirements of section 1902(a)(1) (relating to statewideness), section 1902(a)(10)(B) (relating to comparability), and section 1902(a)(10)(C)(i)(III) (relating to income and resource rules applicable in the community).”)
1
In Olmstead v. L.C. ex rel. Zimring, the Court held that public entities must provide community-based services to persons with disabilities when “the State’s treatment professionals have determined that community placement is appropriate, the transfer from institutional care to a less restrictive setting is not opposed by the affected individual, and the placement can be reasonably accommodated, taking into account the resources available to the State and the needs of others with mental disabilities.” 527 U.S. 581, 587 (1999).
1
Although states must pay for nursing facility services under Medicaid, it is optional for states to pay for home and community-based care. See, e.g., Mary Sowers, Henry Claypool, et al., Streamlining Medicaid Home and Community-Based Services: Key Policy Questions, Kaiser Family Foundation, March 11, 2016, https://www.kff.org/report-section/streamlining-medicaid-home-and-community-based-services-key-policy-questions-issue-brief/.
1
See, e.g., MACPAC, Report to Congress on Medicaid and CHIP: Chapter 4: Access to Home- and Community-Based Services, June 2023, https://www.macpac.gov/wp-content/uploads/2023/06/Chapter-4-Access-to-Home-and-Community-Based-Services.pdf (for information on overall access limitations and budget restrictions).See Alice Burns, Maiss Mohamed, et al., A Look at Waiting Lists for Medicaid Home- and Community-Based Services from 2016 to 2024, Kaiser Family Foundation, October 31, 2024, https://www.kff.org/medicaid/issue-brief/a-look-at-waiting-lists-for-medicaid-home-and-community-based-services-from-2016-to-2024/ (for information about waiting lists across states).
1
M. Christine Tonner and Charlene Harrington, Nursing Facility and Home and Community Based Service Need Criteria in the United States, 22 (4) Home Health Care Serv Q, 65, 2003, https://pubmed.ncbi.nlm.nih.gov/14998282/.
1
See, e.g., Carli Friedman, The Relationship Between Disability Prejudice and Institutionalization of People With Intellectual and Developmental Disabilities, 57 (4) Intellectual and Developmental Disabilities, 263, 2019, https://doi.org/10.1352/1934-9556-57.4.263.
1
See, e.g., AP-NORC Center for Public Affairs Research, The Long Term Care Poll, Long-Term Care in America: Expectations and Preferences for Care and Caregiving, 2016, https://www.longtermcarepoll.org/long-term-care-in-america-expectations-and-preferences-for-care-and-caregiving/ (for long-term care preferences among older adults); MACPAC, Access in Brief: Seniors and Adults with Physical Disabilities, 2024, https://www.macpac.gov/wp-content/uploads/2024/08/Access-in-Brief-Seniors-and-Adults-with-Physical-Disabilities.pdf#xd_co_f=NTJkZTFiOTMtNWJjMi00MjA0LThiNmUtMmY2ZWI3YzU3NGI2~ (for older adults and adults with disabilities).
1
See, MACPAC, Report to Congress on Medicaid and CHIP: Chapter 4: Access to Home- and Community-Based Services, June 2023, https://www.macpac.gov/wp-content/uploads/2023/06/Chapter-4-Access-to-Home-and-Community-Based-Services.pdf.
1
See, Peter Kemper, Randall S. Brown, et al., US Department of Health and Human Services, The Evaluation of the National Long-Term Care Demonstration, 1988, https://aspe.hhs.gov/reports/evaluation-national-long-term-care-demonstration
1
The federal government sponsored a series of experimental programs to test the cost-effectiveness of providing home care instead of institutional care. The largest of these experiments was the National Long-Term Care Channeling Demonstration, which began in 1980. One of the explicit goals of the project was to ensure unpaid care families were already providing was not replaced by government-funded home care: “Channeling was expected to increase the use of formal community-based care by the frail elderly. However, if this led to substitution of formal for informal care, the public sector would then be paying for services otherwise provided by family and friends.” See US Department of Health and Human Services, National Long-Term Care Channeling Demonstration: Summary of Demonstration and Reports, 1987, https://aspe.hhs.gov/reports/national-long-term-care-channeling-demonstration-summary-demonstration-reports-0.
1
“Annually in the United States, about 40 million family caregivers provide an estimated 37 billion hours of care. This unpaid assistance is valued at $470 billion.” See Eric Carlson, Voluntary Means Voluntary: Coordinating Medicaid HCBS with Family Assistance, Justice in Aging, May 2016, https://www.justiceinaging.org/wp-content/uploads/2016/05/Voluntary-Means-Voluntary-Coordinating-Medicaid-HCBS-with-Family-Assistance.pdf.
1
Eileen Borris and Jennifer Klein, Labor on the Home Front: Unionizing Home-Based Care Workers, 17(2) New Labor Forum, 32, 2008, http://www.jstor.org/stable/40342996.
1
Whitney Curry Wimbish, Everything Must Go, 47 The Baffler, 2019, https://thebaffler.com/salvos/everything-must-go-wimbish.
1
See, e.g., Douglas Baynton, Disability and the justification of inequality in American history, 17 (33) The disability studies reader, 33, 2013, https://www.uua.org/files/documents/bayntondouglas/justification_inequality.pdf; Sarah Rose, No right to be idle: The invention of disability, 1840s–1930s, 2017.
1
See, e.g., Joyce Chediac, Disability and Empire: Class, US Imperialism, and the Struggle for Disability Justice, 2024.
1
See, e.g., Gérard Duménil and Dominique Lévy, Capital Resurgent: Chapter 6, 2004; David Harvey, A Brief History of Neoliberalism, 2005; Javier Lopez, Trump’s Big Beautiful Bill is Class War, Liberation News, July 4, 2025, https://liberationnews.org/trumps-big-beautiful-bill-is-class-war/.
1
See, e.g., Trump’s tax law will mostly benefit the rich, while leaving poorer Americans with less, CBO says, The Associated Press, August 11, 2025, https://www.nbcnews.com/politics/congress/trump-tax-law-mostly-benefit-rich-leaving-poorer-americans-less-cbo-rcna224449.
1
See, e.g., Jessica Schubel, Alison Barkoff, et al., History Repeats? Faced with Medicaid Cuts, States Reduced Support for Older Adults and Disabled People, Health Affairs, April 16, 2025, https://www.healthaffairs.org/content/forefront/history-repeats-faced-medicaid-cuts-states-reduced-support-older-adults-and-disabled.
1
Mandate for Leadership: The Conservative Promise, The Heritage Foundation, pp. 283, 462, 2023, https://static.heritage.org/project2025/2025_MandateForLeadership_FULL.pdf
1
See “HCBS Waivers” in the Key Concepts section of this report.
1
For HCBS waiver eligibility, the state must determine that “but for the provision of such services the individuals would be likely to require the level of care provided in a skilled nursing facility or intermediate care facility the cost of which could be reimbursed under the State plan.” 42 U.S.C. § 1396n(c)(1).
1
See, e.g., Mary Killough, Steve Lutzky, et al., Understanding and Improving Nursing Facility Level of Care Criteria to Support Efficiency and Equity, 2024 Home and Community-Based Services conference.
1
“The transformed eligibility guidelines for this program will ensure the right services, to the right people, in the right setting, at the right time.” See Missouri Department of Health and Senior Services, Level of Care Transformation, 2024, https://web.archive.org/web/20240811173827/https://health.mo.gov/seniors/hcbs/loc-transformation.php
1
Miguel Carabantes discusses opacity in artificial intelligence systems as “intentional corporate or institutional concealment of their algorithms” relying on using trade secrets and “technological illiteracy that prevents society from understanding a field as specialized as that of computer programming.” Similar types of opacity are also present in state discussions of LOC algorithms. See Miguel Carabantes, Black-box artificial intelligence: An epistemological and critical analysis, 35 (2) AI & SOCIETY, 309, 2020, https://doi.org/10.1007/s00146-019-00888-w.
1
See, e.g., Paul Longmore, The End of the Beginning: The Disability Rights Movement in the 1970s, Journal of Civil and Human Rights, 2020; Richard Scotch, Politics and Policy in the History of the Disability Rights Movement, The Milbank Quarterly, 1989; Jacob Abudaram, Deinstitutionalization, Disease, and the HCBS Crisis, Michigan Law Review, 2023. See also Jordan Conrad, On intellectual and developmental disabilities in the United States: A historical perspective, Journal of Intellectual Disabilities, 2020 (for a history of how disabilities have been viewed in the United States).
1
See, e.g., Samuel R. Bagenstos, The Past and Future of Deinstitutionalization Litigation, Law & Economics
1
See, e.g., Paul Longmore, The End of the Beginning: The Disability Rights Movement in the 1970s, Journal of Civil and Human Rights, 2020; Chava Willig Levy and the Independent Living Institute, A People’s History of the Independent Living Movement, 1998, https://www.independentliving.org/docs5/ILhistory.html.
1
The 1967 Social Security Amendments increased regulations for nursing facilities and the 1968 Moss Amendments increased standardization of nursing facilities. See Institute of Medicine (US) Committee on Nursing Home Regulation, Improving the Quality of Care in Nursing Homes: History of Federal Nursing Home Regulation, 1986, https://www.ncbi.nlm.nih.gov/books/NBK217552/.
1
Pamela Doty and U.S. Department of Health and Human Services, Cost-Effectiveness of Home and Community-Based Long-Term Care Services, June 2000, https://aspe.hhs.gov/sites/default/files/private/pdf/73916/costeff.pdf.
1
H.R.3982, 97th Congress (1981-1982).
1
Cynthia Shirk, Rebalancing Long-Term Care: The Role of the Medicaid HCBS Waiver Program, National Health Policy Forum, 2006.
1
Gary Clarke describes how, “Deinstitutionalization became the ideal social reform; it permitted liberal politicians to free mental patients, and at the same time allowed conservative politicians to save millions of dollars.” See Gary Clarke, In Defense of Deinstitutionalization, The Milbank Quarterly, 1979.
1
“State and federal policymakers have considered the expansion of noninstitutional services a mechanism that both increases client welfare and lowers costs. That is, individuals generally prefer care in the home or community, and for certain individuals with less intensive care needs, it may be possible to provide lower per capita cost care in the home or community relative to a nursing facility. However, the historic institutional bias in long-term care coverage relates partially to a perceived moral hazard problem (or woodwork effect) whereby publicly financed noninstitutional services substitute for informal services previously provided by family members and friends.” David Grabowski, The cost-effectiveness of non-institutional long-term care services: Review and synthesis of the most recent evidence, 63 Medical Care Research and Review, 13, 2006, https://pubmed.ncbi.nlm.nih.gov/16686071/.
1
See, e.g., Douglas Baynton, Disability and the justification of inequality in American history, 17(33) The disability studies reader, 33, 2013; Sarah Rose, No right to be idle: The invention of disability, 1840s–1930s, 2017.
1
See Eileen Borris and Jennifer Klein, Labor on the Home Front: Unionizing Home-Based Care Workers, 17 (2) New Labor Forum, 32, 2008, http://www.jstor.org/stable/40342996. As of 2022, women of color made up 53 percent of the direct care workforce, according to research from PHI. See Stephen McCall and Kezia Scales, Direct Care Worker Disparities: Key Trends and Challenges, February 8, 2022, https://www.phinational.org/resource/direct-care-worker-disparities-key-trends-and-challenges/.
1
“Annually in the United States, about 40 million family caregivers provide an estimated 37 billion hours of care. This unpaid assistance is valued at $470 billion.” See Eric Carlson and Justice in Aging, Voluntary Means Voluntary: Coordinating Medicaid HCBS with Family Assistance, May 2016, https://www.justiceinaging.org/wp-content/uploads/2016/05/Voluntary-Means-Voluntary-Coordinating-Medicaid-HCBS-with-Family-Assistance.pdf.
1
See, e.g., Jessica Schubel, Alison Barkoff, et a., History Repeats? Faced with Medicaid Cuts, States Reduced Support for Older Adults and Disabled People, Health Affairs, April 16, 2025, https://www.healthaffairs.org/content/forefront/history-repeats-faced-medicaid-cuts-states-reduced-support-older-adults-and-disabled.
1
Participants in a March 2021 workshop on long-term supports and services, co-hosted by Upturn and the Center for Democracy and Technology, cited autonomy in decision-making about where to direct service budgets as something they would like to change about benefits programs.
1
Jennifer Lav and National Health Law Program, A Change Worth Investing In – Medicaid Home and Community Based Services, 2021, https://healthlaw.org/a-change-worth-investing-in-medicaid-home-and-community-based-services/.
1
There is a growing body of literature surrounding accountability, transparency, and regulatory issues with the government’s increasing reliance on automated systems developed by the private sector. See, e.g., Danielle Citron and Frank Pasquale, The scored society: Due process for automated predictions, 89 (1) Washington Law Review, 1, 2014; Ryan Calo and Danielle Citron, The Automated Administrative State: A Crisis of Legitimacy, 70 (4) Emory Law Journal, 797, 2021; Kate Crawford and Jason Schultz, AI Systems as State Actors, 119 (7) Columbia Law Review, 1941, 2019; Miguel Carabantes, Black-box artificial intelligence: An epistemological and critical analysis, 35 (2) AI & SOCIETY, 309, 2020.
1
For example, in an Idaho lawsuit, the American Association on Intellectual and Developmental Disabilities alleged that the manual for their Supports Intensity Scale for Adults assessment was proprietary and thus could not be produced to the class of plaintiffs. Declaration of Alan W. Foutz in Support of IDHW’s Motion to Preclude Dissemination of the SIS-A User’ Manual to Class Members, K.W. v. Armstrong, No. 1:12-cv-00022-BLW (D. Idaho 2023), https://storage.courtlistener.com/recap/gov.uscourts.idd.29058/gov.uscourts.idd.29058.539.4.pdf; Exhibit A to the Declaration of Alan W. Foutz, K.W. v. Armstrong, No. 1:12-cv-00022-BLW (D. Idaho 2023), https://storage.courtlistener.com/recap/gov.uscourts.idd.29058/gov.uscourts.idd.29058.539.5_1.pdf. The organization even threatened not to renew its contract with the state if the manual was not released without sufficient protections. Exhibit B to the Declaration of Alan W. Foutz, K.W. v. Armstrong, No. 1:12-cv-00022-BLW (D. Idaho 2023), https://storage.courtlistener.com/recap/gov.uscourts.idd.29058/gov.uscourts.idd.29058.539.6.pdf.
1
See Appendix B: Public Records Requests Denials.
1
We used two methods to compare LOC criteria across states, looking at publicly available and self-reported information, as well as information we received through records requests and our work with state advocates. We reviewed the LOC algorithms for the five states for which we were able to obtain the actual algorithm logic, all of which use the interRAI HC assessment. We also reviewed waiver applications, available on the CMS website (https://www.medicaid.gov/medicaid/section-1115-demo/demonstration-and-waiver-list), for at least one 1915(c) elderly and/or physically disabled waiver program from all 50 states to compare the LOC criteria as self-reported by each state for the given waiver program. It is important to note that states’ actual eligibility determinations processes may vary significantly from what is reported in their waiver application.
1
March 2021 workshop on long-term supports and services, co-hosted by Upturn and the Center for Democracy and Technology.
1
An example from Minnesota during the rollout of a new assessment tool showed the level of anxiety individuals feel in knowing how to respond to assessment questions to make sure that they receive care. One mother, whose son received an arbitrary budget cut, worried about the adequacy of her response to the assessor on her son’s behalf, saying “maybe I didn’t advocate hard enough for him during that assessment.” Glenn Howatt and Chris Serres, High-stakes assessments can upend lives of Minnesota families with disabilities, The Minnesota Star Tribune, October 7, 2019, https://www.startribune.com/high-stakes-assessments-can-upend-lives-of-minnesota-families-with-disabilities/558453432.
1
See, e.g., Amber Christ and Natalie Kean, An Equity Framework for Evaluating and Improving Medicaid Home and Community-Based Services, Justice in Aging, June 2023, https://justiceinaging.org/wp-content/uploads/2023/06/An-HCBS-Equity-Framework.pdf.
1
Eleven of the 41 waiver applications we reviewed specified use of the interRAI HC. Two states used the Minimum Data Set-Home Care tool and two used the Universal Assessment Instrument. The remaining 26 states use different tools, including various state forms, custom state tools, or other vendor-provided tools. However, waiver applications are not necessarily the most accurate source for what states are doing in reality. Other sources show a greater number of states using interRAI tools. As of 2020, 24 states were using interRAI’s Home Care assessment, according to a vendor report for Nebraska’s Medicaid agency. See Optumas, Nebraska Department of Health and Human Services Nursing Facility Level of Care (NF LOC) Assessment Tool and Criteria: Recommendation Report, p. 24, June 29, 2020.
1
See Florida State University College of Medicine, ADvancing interRAI: Using Better Data, Better, April 8, 2024, https://med.fsu.edu/news/bssm/advancing-interrai-using-better-data-better/mon-04082024-0822#:~:text=ADvancing%20interRAI%2C%20a%20new%20initiative,eligibility%20and%20establishing%20service%20packages.
1
John P. Hirdes, Coline van Everdingen, et al., The interRAI Suite of Mental Health Assessment Instruments: An Integrated System for the Continuum of Care, 10 Frontiers in psychiatry, 926, 2020, https://pmc.ncbi.nlm.nih.gov/articles/PMC6978285/#s2.
1
Minnesota’s assessment, MnCHOICES, is an example of a customized universal assessment created by a state working with private vendors. A “universal” assessment means a single assessment that can be used for various populations and waiver types, rather than using different assessments for each program. While universal assessments are often touted as more “fair” and “person-centered” because they start with a person rather than a program, they still have the same limitations as any standardized assessment, are used to target eligibility, and often have issues with lack of transparency due to private contracting. See Minnesota Department of Human Services, MnCHOICES, 2025, https://mn.gov/dhs/partners-and-providers/news-initiatives-reports-workgroups/long-term-services-and-supports/mnchoices/; Penny Black and Kathy Leitch, Analysis of State Approaches to Implementing Standardized Assessments, p. 38, April 2012, https://www.chhs.ca.gov/wp-content/uploads/2017/06/Committees/Olmstead-Advisory/Material-Archive/The-SCAN-Foundation-Funded-Report-on-Uniform-Assessments.pdf.
1
interRAI, “About interRAI,” https://interrai.org/about-interrai/.
1
For example, reliability for an assessment can include test-retest reliability, inter-rater reliability, and internal consistency. Validity types include construct validity, content validity, face validity, and criterion validity.
1
A 2008 study found the interRAI HC to have substantial reliability based on Landis and Koch’s convention for interpreting kappa values (a measure of inter-rater agreement). See John P Hirdes, Gunnar Ljunggren, et al., Reliability of the interRAI suite of assessment instruments: a 12-country study of an integrated health information system, 8 BMC Health Services Research, 277, 2008, https://pmc.ncbi.nlm.nih.gov/articles/PMC2631461/.
1
The study compared questions on the interRAI HC to the Barthel Activities of Daily Living Index, the Instrumental Activities of Daily Living of Lawton, and the Mini Mental State Examination. See Francesco Landi, Ennio Tua, et al., Minimum Data Set for Home Care: A Valid Instrument to Assess Frail Older People Living in the Community, 38 (12) Medical Care, 1184, 2000, https://journals.lww.com/lww-medicalcare/abstract/2000/12000/minimum_data_set_for_home_care__a_valid_instrument.5.aspx.
1
See, e.g., State of Iowa Department of Health and Human Services, Core Standardized Assessments: Molina Onboarding, October 2022, https://www.documentcloud.org/documents/26053756-hcbs-core-standardized-assessments-new/.
1
For example, interRAI used data from Nebraska and another midwestern state to analyze changes in eligibility across various dimensions including demographics and diagnoses to assess the new algorithm. Optumas used this interRAI analysis to discuss potential changes with the state agency. See Optumas, Nebraska Division of Developmental Disabilities Home- and Community-Based Services Redesign Project, interRAI HC Assessment and Implementation Support, p. 17, October 25, 2021, https://www.documentcloud.org/documents/26053849-ne-hcbs-adult-assessment-implementation-support-20211025-final-to-state/. When Missouri published a draft version of its proposed new algorithm for public comment in 2018, Upturn worked with Legal Services of Eastern Missouri to evaluate the impact of the proposed changes finding that an estimated 66 percent of people who were then-currently eligible would become ineligible under the redesigned system. After advocates shared this finding with the state agency, the agency worked with a consultant, Mercer, to evaluate a subsequent version of the proposed algorithm. Mercer found that the eligible population would decrease by 19 percent. See Mercer, Missouri Department of Health and Senior Services: Nursing Facility Level of Care Algorithm Analysis, p. 5, January 24, 2020, https://drive.google.com/file/d/15jm4-Cd7ZPgRmDkn6dglfujW0xai79bA/view. Missouri did not report any testing of the final version of the algorithm, which was implemented in October 2024. See Benefits Tech Advocacy Hub, Missouri Medicaid Home and Community Based Services Eligibility Issues, https://www.btah.org/case-study/missouri-medicaid-home-and-community-based-services-eligibility-issues.html.
1
Earlier research has similarly found wide variation in how states determine the institutional level of care but arrived at different recommendations for how to address this. See Melanie Thomasson, Mary James, Brant Fries, Using Standardized Date to Compare Access to Long-Term Services and Supports in Five US States, Volume 1 Innovation in Aging Issue suppl_1 Page 678, July 2017, https://doi.org/10.1093/geroni/igx004.2413; Melanie Thomasson, Steve Lutzky, Mary Killough, Bea Rector, Bonnie Silva, Understanding and Improving Nursing Facility Level of Care to Support Efficiency and Equity, Home and Community-Based Services Conference, 2024.
1
Missouri Department of Health and Senior Services, Level of Care Transformation, https://web.archive.org/web/20241204234508/https://health.mo.gov/seniors/hcbs/loc-transformation.php.
1
Mercer Government Human Services Consulting and the National Association of States United for Aging and Disabilities, Nebraska Long-Term Care Redesign Plan - Draft, March 7, 2017, https://dhhs.ne.gov/Documents/Long-Term%20Care%20Redesign%20Draft%20by%20Mercer%20Health%20Benefits,%20Inc.pdf.
1
Michigan, for example, emphasizes the consistency and reliability of the tools used for eligibility determinations. See Michigan Department of Health and Human Services, Medicaid Provider Manual, 2019, https://www.documentcloud.org/documents/26053823-medicaidprovidermanualfound-online/. In Iowa, an onboarding presentation that covered the assessment process describes it as a way to gather, “objective information to guide service planning.” See Iowa Health and Human Services, Core Standardized Assessments, 2022, https://www.documentcloud.org/documents/26053756-hcbs-core-standardized-assessments-new/.
1
Here, we emphasize the systemic issue caused by widespread underfunding of home and community-based services, which leads state agencies to depoliticize eligibility determinations through technical processes. Many individual state officials and state agencies may have the best intentions, doing what they can to maximize people’s benefits under budget constraints. The problem is not with the intentions of state agency officials, but rather with the limitations caused by the budgets themselves.
1
See, e.g., Declaration of Alan W. Foutz in Support of IDHW’s Motion to Preclude Dissemination of the SIS-A User’ Manual to Class Members, K.W. v. Armstrong, No. 1:12-cv-00022-BLW (D. Idaho 2023), https://storage.courtlistener.com/recap/gov.uscourts.idd.29058/gov.uscourts.idd.29058.539.4.pdf; Exhibit A to the Declaration of Alan W. Foutz, K.W. v. Armstrong, No. 1:12-cv-00022-BLW (D. Idaho 2023), https://storage.courtlistener.com/recap/gov.uscourts.idd.29058/gov.uscourts.idd.29058.539.5_1.pdf; Exhibit B to the Declaration of Alan W. Foutz, K.W. v. Armstrong, No. 1:12-cv-00022-BLW (D. Idaho 2023), https://storage.courtlistener.com/recap/gov.uscourts.idd.29058/gov.uscourts.idd.29058.539.6.pdf
1
Optumas, Nebraska Division of Developmental Disabilities Home- and Community-Based Services Redesign Project, interRAI HC Assessment and Implementation Support, p. 41, October 25, 2021, https://www.documentcloud.org/documents/26053849-ne-hcbs-adult-assessment-implementation-support-20211025-final-to-state/.
1
Government of the District of Columbia Department of Health Care Finance, FY 18-19 Oversight Report to DC Council, p. 133, April 2019, https://dccouncil.gov/wp-content/uploads/2019/04/dhcf.pdf.
1
Government of the District of Columbia Department of Health Care Finance, FY 18-19 Oversight Report to DC Council, p. 133, April 2019, https://dccouncil.gov/wp-content/uploads/2019/04/dhcf.pdf.
1
Department of Health Care Finance, Notice of Emergency and Proposed Rulemaking - Governing Long Term Care Services and Supports Assessment Process, 66 (7) DC Register, 1, 2019, https://www.dcregs.dc.gov/Common/NoticeDetail.aspx?NoticeId=N0078880.
1
Department of Health Care Finance, Notice of Second Emergency and Proposed Rulemaking - Governing Long Term Care Services and Supports Assessment Process, 67 (37) DC Register, pp. 6–7, 2020, https://www.dcregs.dc.gov/Common/NoticeDetail.aspx?NoticeId=N0097527.
1
Department of Health Care Finance, Notice of Second Emergency and Proposed Rulemaking - Governing Long Term Care Services and Supports Assessment Process, 67 (37) DC Register, pp. 6–7, 2020, https://www.dcregs.dc.gov/Common/NoticeDetail.aspx?NoticeId=N0097527.
1
Department of Health Care Finance, Notice of Second Emergency and Proposed Rulemaking - Governing Long Term Care Services and Supports Assessment Process, 67 (37) DC Register, pp. 6–7, 2020, https://www.dcregs.dc.gov/Common/NoticeDetail.aspx?NoticeId=N0097527.
1
Government of the District of Columbia Department of Health Care Finance, FY 18-19 Oversight Report to DC Council, pp. 138–140, April 2019, https://dccouncil.gov/wp-content/uploads/2019/04/dhcf.pdf.
1
Department of Health Care Finance, Notice of Second Emergency and Proposed Rulemaking - Governing Long Term Care Services and Supports Assessment Process, 67 (37) DC Register, 7, 2020, https://www.dcregs.dc.gov/Common/NoticeDetail.aspx?NoticeId=N0097527.
1
Department of Health Care Finance, Notice of Second Emergency and Proposed Rulemaking - Governing Long Term Care Services and Supports Assessment Process, 67 (37) DC Register, 7, 2020, https://www.dcregs.dc.gov/Common/NoticeDetail.aspx?NoticeId=N0097527.
1
Department of Health Care Finance, Notice of Final Rulemaking - Governing Long Term Care Services and Supports Assessment Process, 68 (15) DC Register, 2, 2021, https://www.dcregs.dc.gov/Common/NoticeDetail.aspx?NoticeId=N105822.
1
Department of Health Care Finance, Notice of Second Emergency and Proposed Rulemaking - Governing Long Term Care Services and Supports Assessment Process, 67 (37) DC Register, 8, 2020, https://www.dcregs.dc.gov/Common/NoticeDetail.aspx?NoticeId=N0097527.
1
Department of Health Care Finance, Notice of Second Emergency and Proposed Rulemaking - Governing Long Term Care Services and Supports Assessment Process, 67 (37) DC Register, 8, 2020, https://www.dcregs.dc.gov/Common/NoticeDetail.aspx?NoticeId=N0097527.
1
Notably, at the same time, the legislature also lowered the cost cap for personal care services from 100 percent of the cost of nursing facility care to 60 percent. The cost cap limits the amount of services people can get through Missouri’s HCBS program, so when the cost cap was reduced, people experienced a reduction in the hours of care they could get in their home. The highest-need participants went from 6 hours of care per day to 4 hours of care per day. Missouri Alliance for Home Care, RESTORE the 60% CAP to 100% in CONSUMER DIRECTED SERVICES PROGRAM, Talking Points, https://homecaremissouri.org/mahc/documents/TALKINGPOINTS-CDS60percent.pdf.
1
Missouri Department of Health and Senior Services, Memorandum for all Home and Community Based Care Providers, December 26, 2018, https://web.archive.org/web/20231001125619/https://health.mo.gov/seniors/hcbs/pmvmdocs/PM-18-22VM-18-22.pdf.
1
The Department of Health and Senior Services first introduced an emergency amendment in August 2017 in response to the legislature changing the LOC score required for eligibility. The department then published proposed rules in February 2021 and November 2021. The final rule was published on March 1, 2022 and went into effect March 31 of that year. See John R. Ashcroft, Emergency Amendment in Missouri Register, 42 (16) Missouri Register, 2017, https://www.sos.mo.gov/CMSImages/AdRules/moreg/2017/v42n16Aug15/v42n16a.pdf; Proposed Rule in Missouri Register, 46 (4) Missouri Register, 2021, https://www.sos.mo.gov/CMSImages/AdRules/moreg/2021/v46n4Feb16/v46n4b.pdf; Proposed Rule in Missouri Register, 46 (22) Missouri Register, 2021, https://www.sos.mo.gov/CMSImages/AdRules/moreg/2021/v46n22Nov15/v46n22c.pdf; Order of Rulemaking in Missouri Register, 47 (5) Missouri Register, 2022, https://www.sos.mo.gov/CMSImages/AdRules/moreg/2022/v47n5March1/v47n5b.pdf.
1
Go Long Consulting, Technical Assistance Report to The State of Missouri Department of Health and Senior Services on the Nursing Facility (NF) Level of Care (LOC) Transformation, December 2018, https://health.mo.gov/seniors/hcbs/pdf/levelofcaretransformation.pdf.
1
Benefits Tech Advocacy Hub, Missouri Medicaid Home and Community Based Services Eligibility Issues, https://www.btah.org/case-study/missouri-medicaid-home-and-community-based-services-eligibility-issues.html.
1
Legal Services of Eastern Missouri and the Benefits Tech Advocacy Hub, Analysis of Missouri’s New Eligibility Process for Home and Community Based Services, September 2024, https://docs.google.com/document/d/1C-XTFFwMTO8NhUzHaVzzu-5H48li-0K5Zi0y-FDlySs.
1
Missouri Department of Health and Senior Services, LOC Transformation Training Opportunities webinar, September 20, 2024, https://stateofmo.webex.com/recordingservice/sites/stateofmo/recording/8d5b5ed15984103dbfd6d6c4b67e734f/playback.
1
Missouri Department of Health and Senior Services, LOC Transformation Training Opportunities webinar, 1:46:40, September 20, 2024, https://stateofmo.webex.com/recordingservice/sites/stateofmo/recording/8d5b5ed15984103dbfd6d6c4b67e734f/playback.
1
Missouri Department of Health and Senior Services, LOC Transformation Training Opportunities webinar, September 20, 2024, https://stateofmo.webex.com/recordingservice/sites/stateofmo/recording/8d5b5ed15984103dbfd6d6c4b67e734f/playback.
1
“When the waiver level of care instrument/tool differs from the instrument/tool used to determineinstitutional level-of-care, 42 CFR §441.303(c)(1) requires the state to describe how and why theydiffer and explain how the outcome of the level of care determination under the waiver is reliable,valid, and fully comparable to the outcome for institutional evaluation.” See Application for a §1915(c) Home and Community-Based Waiver: Instructions, Technical Guide and Review Criteria, Centers for Medicare & Medicaid Services, January 2019, https://wms-mmdl.cms.gov/WMS/help/35/Instructions_TechnicalGuide_V3.6.pdf.
1
The Division of Developmental Disabilities was already managing the developmental disabilities waivers and also took on administration of the state’s Traumatic Brain Injury waiver. See, Optumas, Nebraska Division of Developmental Disabilities Home- and Community-Based Services Redesign Project, interRAI HC Assessment and Implementation Support, 4, October 25, 2021, https://www.documentcloud.org/documents/26053849-ne-hcbs-adult-assessment-implementation-support-20211025-final-to-state/.
1
Optumas, Nebraska Division of Developmental Disabilities Home- and Community-Based Services Redesign Project, interRAI HC Assessment and Implementation Support, 4, October 25, 2021, https://www.documentcloud.org/documents/26053849-ne-hcbs-adult-assessment-implementation-support-20211025-final-to-state/.
1
Optumas, Nebraska Department of Health and Human Services Nursing Facility Level of Care (NF LOC) Assessment Tool and Criteria: Recommendation Report, June 29, 2020, https://www.documentcloud.org/documents/26054257-ne-nf-loc-recommendation-report-2020-06-29-final-to-state/.
1
Nebraska Department of Health and Human Services, 471 NAC 12, 12-003.02 Nursing Facility Level of Care Criteria for Adults, December 19, 2018, http://govdocs.nebraska.gov/epubs/H8310/R471.0012-2018.pdf.
1
Nebraska Department of Health and Human Services, 471 NAC 44, 44-002.02 Nursing Facility Level of Care Determination for Adults, May 11, 2022, https://govdocs.nebraska.gov/epubs/H8900/R471.0044-2022.pdf.
1
Optumas, Nebraska Division of Developmental Disabilities Home- and Community-Based Services Redesign Project, interRAI HC Assessment and Implementation Support, p. 45, October 25, 2021, https://www.documentcloud.org/documents/26053849-ne-hcbs-adult-assessment-implementation-support-20211025-final-to-state/.
1
“For example, putting your ADLs at “supervision plus” is not typical, but that is what you all have. But a lot of these differences are due to policy characteristics that we are not aware of on our end.” Optumas, Nebraska Division of Developmental Disabilities Home- and Community-Based Services Redesign Project, interRAI HC Assessment and Implementation Support, p. 46, October 25, 2021, https://www.documentcloud.org/documents/26053849-ne-hcbs-adult-assessment-implementation-support-20211025-final-to-state/.
1
Optumas, Nebraska Division of Developmental Disabilities Home- and Community-Based Services Redesign Project, interRAI HC Assessment and Implementation Support, p. 46, October 25, 2021, https://www.documentcloud.org/documents/26053849-ne-hcbs-adult-assessment-implementation-support-20211025-final-to-state/.
1
Optumas, Nebraska Division of Developmental Disabilities Home- and Community-Based Services Redesign Project, interRAI HC Assessment and Implementation Support, p. 46, October 25, 2021, https://www.documentcloud.org/documents/26053849-ne-hcbs-adult-assessment-implementation-support-20211025-final-to-state/.
1
Optumas, Nebraska Division of Developmental Disabilities Home- and Community-Based Services Redesign Project, interRAI HC Assessment and Implementation Support, p. 41, October 25, 2021, https://www.documentcloud.org/documents/26053849-ne-hcbs-adult-assessment-implementation-support-20211025-final-to-state/.
1
CMS waiver applications ask states to “fully specify the level of care criteria that are used to evaluate and reevaluate whether an individual needs services through the waiver” and to “specify the level of care instrument/tool that is employed.” Despite this requirement, most states do not provide a detailed description of the criteria. While you are unlikely to get the full logic of the algorithm through even the most complete response to this question, you can check your state’s waiver application for more information on LOC criteria. If your state is applying for a new waiver or amending an existing waiver, you can also provide comments on that application or amendment, pushing the state to provide more details about the LOC criteria. A database of state waivers is available on the CMS website. Note this information is self-reported and may be out-of-date or otherwise inaccurate. See Centers for Medicare and Medicaid Services, State Waivers List, https://www.medicaid.gov/medicaid/section-1115-demo/demonstration-and-waiver-list.
1
Government of the District of Columbia, Department of Health Care Finance, FY 18-19 Oversight Report to DC Council, p. 138–140, February 4, 2019, https://dccouncil.gov/wp-content/uploads/2019/04/dhcf.pdf.
1
See, e.g., Benefits Tech Advocacy Hub, Idaho Medicaid Home and Community Based Services Care Cuts, https://www.btah.org/case-study/idaho-medicaid-home-and-community-based-services-care-cuts.html.
1
Benefits Tech Advocacy Hub, Public Records Request Guide, https://www.btah.org/resources/public-records-request-guide.html.
1
“There is no authority for the proposition . . . that the federal copyright laws and local trade secret laws trump the federal Medicaid statute and regulations.” Salazar v. District of Columbia, Civil Action No. 93-452 (GK) (D.D.C. 2009), pg. 4 (noting that both Medicaid beneficiaries and their counsel are entitled to know what criteria is being utilized to make Medicaid determinations and specifically referencing the “Interqual Criteria” and the provision of PDN services, and explicitly recognizing that University Legal Services requires access to the criteria in order to advise clients on entitlement to Medicaid services); see also L.S. v. Deliah, 2012 WL 12911052 (E.D.N.C. March 29, 2012) at 13 (granting preliminary injunction for plaintiff class of Medicaid beneficiaries in part because state Medicaid agency and managed care company used assessment tools to reduce home and community-based services without explaining “the significance of the [assessment] score or how to challenge it.”).
1
Ly Xīnzhèn Zhǎngsūn Brown, Michelle Richardson, et al., Challenging the Use of Algorithm-driven Decision-making in Benefits Determinations Affecting People with Disabilities, Center for Democracy and Technology, October 21, 2020, https://cdt.org/insights/report-challenging-the-use-of-algorithm-driven-decision-making-in-benefits-determinations-affecting-people-with-disabilities/.
1
Fill out the technical assistance request form here: https://www.btah.org/how-to-be-involved.html.
1
See, e.g., Benefits Tech Advocacy Hub, Arkansas Medicaid Home and Community Based Services Hours Cuts, https://www.btah.org/case-study/arkansas-medicaid-home-and-community-based-services-hours-cuts.html; Benefits Tech Advocacy Hub, North Carolina Medicaid Home and Community Based Services Care Cuts, https://www.btah.org/case-study/north-carolina-medicaid-home-and-community-based-services-care-cuts.html.
1
Note: Legal services organizations that receive federal funding through the Legal Services Corporation are prohibited from filing class action lawsuits, as well as from organizing and political activity, due to restrictions, rooted in anti-union, anti-collective action politics. The 1996 congressional appropriations bill prohibited organizing and included an anti-solicitation provision that came from trying to prevent farm-worker organizing. Legal Services Corporation, LSC Restrictions and Other Funding Sources, https://www.lsc.gov/about-lsc/laws-regulations-and-guidance/lsc-restrictions-and-other-funding-sources.
1
See, e.g., Benefits Tech Advocacy Hub, Missouri Medicaid Home and Community Based Services Eligibility Issues, https://www.btah.org/case-study/missouri-medicaid-home-and-community-based-services-eligibility-issues.html.
1
Ly Xīnzhèn Zhǎngsūn Brown, Michelle Richardson, et al., Challenging the Use of Algorithm-driven Decision-making in Benefits Determinations Affecting People with Disabilities, Center for Democracy and Technology, October 21, 2020, https://cdt.org/insights/report-challenging-the-use-of-algorithm-driven-decision-making-in-benefits-determinations-affecting-people-with-disabilities/.
Related Work
Our paper on how entities that use algorithmic systems in traditional civil rights domains like housing, employment, and credit should have a duty to search for and implement less discriminatory algorithms (LDAs).
Across the FieldA follow up on the July 13, 2021 letter sent to Assistant Attorney General Kristen Clarke, then-Secretary of Labor Martin Walsh, and then-OFCCP Director Jenny Yang titled Addressing Technology’s Role in Hiring Discrimination (the “2021 letter”) and the “Automated systems, including artificial intelligence (AI)” section of the October 26, 2023 letter sent to the EEOC.
Labor and Employment Jobs and HiringSpecific recommendations on implementing the recently-signed Executive Order on Safe, Secure, and Trustworthy Development and Use of Artificial Intelligence (EO 14110).
Across the Field